Drug Interactions – Spot Risks, Stay Safe
Ever taken two medicines and wondered if they might be fighting each other? That’s a drug interaction. It’s when one drug changes how another works, making one less effective, causing side effects, or even a serious health problem. Knowing the basics can save you from headaches, extra doctor visits, or worse.
Why Drug Interactions Happen
Our bodies break down meds with enzymes, mainly in the liver. Some drugs boost or block these enzymes, speeding up or slowing down the breakdown of another drug. When the timing is off, the second drug can pile up to unsafe levels or disappear too fast to help. Interactions also show up when medicines affect the same organ, like the heart or stomach, or when they share the same chemical pathway. Even foods, alcohol, and herbal supplements can join the mix and tip the balance.
A common example is mixing a blood thinner like warfarin with an antibiotic such as azithromycin. The antibiotic can raise warfarin levels, increasing bleeding risk. Another everyday combo is taking a cold medicine that contains pseudoephedrine with a stimulant like caffeine – you might feel jittery or get a fast heart rate. Knowing these patterns helps you ask the right questions before you start a new prescription.
Easy Ways to Check Interactions
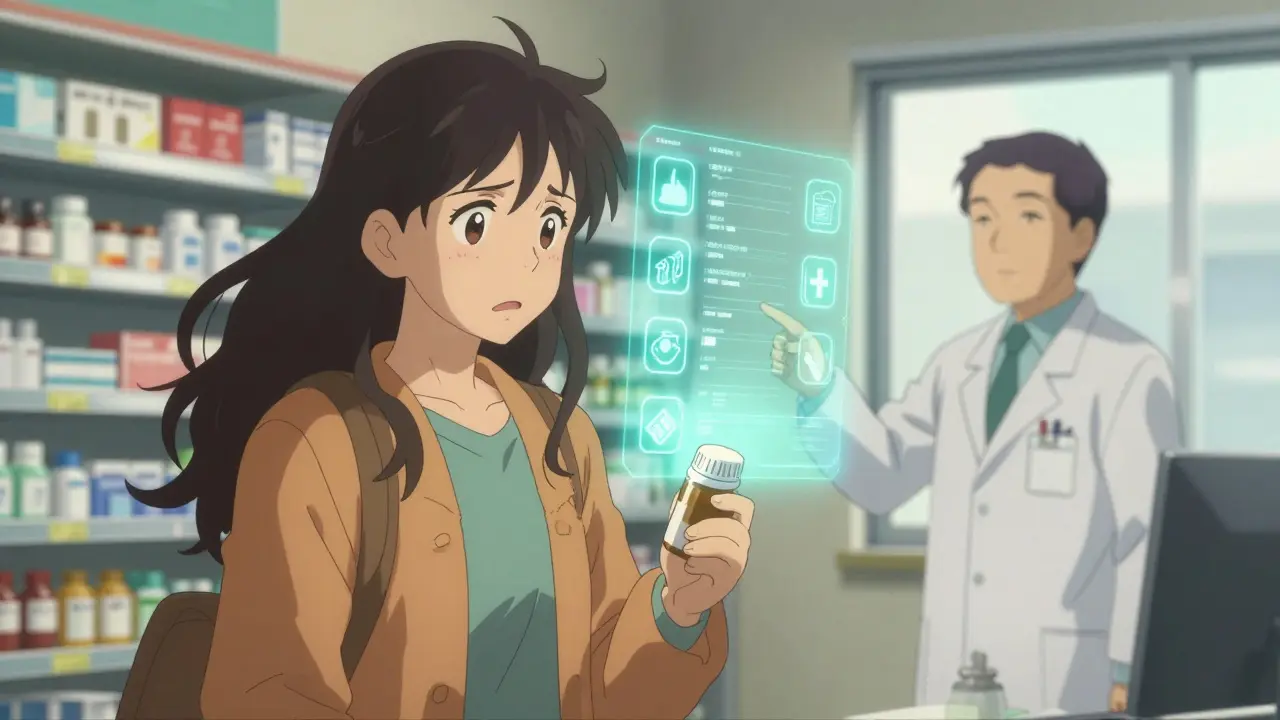
First, always share a complete medication list with any doctor or pharmacist. That list includes prescription drugs, over‑the‑counter pills, vitamins, and herbal products. A quick chat can catch obvious clashes. Second, use a reliable online drug interaction checker. Many pharmacy sites and health portals let you type in the names and see a clear warning if something doesn’t match.
When you get a new prescription, read the patient information leaflet. It usually lists major drugs to avoid. If the warning feels vague, type the drug name into a trusted checker and see which classes it interacts with. Look for color‑coded alerts – red means high risk, orange is moderate, and green is low. If you see a red flag, call your prescriber right away.
Timing can matter too. Some drugs are safe if you separate them by a few hours. For instance, taking calcium supplements at the same time as a thyroid pill can reduce absorption of the thyroid medication. Splitting the doses by at least two hours often solves the problem.
Finally, keep an eye on how you feel. New dizziness, nausea, rash, or unusual tiredness after adding a drug could be a sign of an interaction. Report these symptoms early – a quick adjustment can prevent bigger issues.
Bottom line: drug interactions are common, but they’re also preventable. Keep a current medication list, use a checker, talk openly with your health team, and watch for changes in your body. With these simple steps, you’ll stay in control of your treatment and avoid nasty surprises.
A Beginner’s Guide to Medication Safety for First-Time Patients
Learn how to take medications safely as a first-time patient. Avoid common errors, understand storage, interactions, and dosing with practical steps backed by CDC, FDA, and pharmacy experts.
Learn more...Combining Multiple Heart Medications: Safe and Unsafe Drug Combinations
Combining multiple heart medications can be dangerous due to drug interactions that reduce effectiveness or cause life-threatening side effects. Learn which combinations to avoid and how to stay safe.
Learn more...Warfarin and Type 2 Diabetes: Navigating Complex Drug Interactions for Better INR Control
Warfarin and type 2 diabetes often collide in everyday clinical practice, and the drug interactions can send INR readings on a wild ride. This article digs deep into how antidiabetic medications impact warfarin therapy and what clinicians need to watch for. You'll get real-world strategies for managing INR fluctuations, plus tips to help keep things stable for your patients. Learn about which medications present the biggest challenges and discover straightforward solutions you can use in your next clinic session. Perfect for doctors, pharmacists, and any healthcare professional juggling these two chronic conditions.
Learn more...