The INR Rollercoaster: Why Warfarin and Type 2 Diabetes Don’t Always Play Nice
Mixing warfarin with type 2 diabetes isn’t just common—it’s practically unavoidable. In Australia, about 7% of adults live with type 2 diabetes, and warfarin has long been the go-to blood thinner for managing clots, prosthetic valves, and good old-fashioned atrial fibrillation. But here’s the kicker: diabetics on warfarin are way more vulnerable to erratic INR swings, and it all comes down to unexpected drug interactions.
Why does this happen? Antidiabetic agents like metformin, sulfonylureas, SGLT2 inhibitors, and insulin each tweak the way your body handles warfarin. Some mess with how liver enzymes chew through the drug. Others mess with the gut flora or compete for plasma proteins, booting warfarin off its usual seat and upping its blood-thinning effect. Sometimes, those shifts aren’t just academic—they change whether your patient walks away bruise-free or winds up with a trip to the emergency department. Not fun.
Let’s start with metformin, the so-called gentle giant of diabetes care. For most patients, it doesn’t put warfarin on a seesaw—unless there’s a sudden stop or dose change, which can subtly goose INR readings higher than expected. The real wildcards are sulfonylureas (think gliclazide, glipizide). These drugs don’t just kickstart the pancreas—they compete with warfarin for albumin binding. That’s a catfight for dominance, and warfarin wins by flooding the system and pushing INR levels upwards. No wonder so many GPs see wild INRs after a new diabetes script gets added to the mix.
Insulin isn’t exactly an innocent bystander, either. Sure, its interaction is less direct, but big swings in blood glucose—especially hypoglycemic episodes—can lead to stress responses, infections, or sudden changes in diet. All of these flip INR readings for a loop. Patients who land in hospital with a busted foot ulcer or flu and suddenly need more insulin can swing from sub-therapeutic to sky-high INR overnight.
SGLT2 inhibitors (like empagliflozin) and DPP-4 inhibitors (like sitagliptin) are the newest faces in the room, and the data isn’t as robust, but a few real-world audits out of Sydney and Melbourne clinics point to a trend: patients switched from older agents to these new meds sometimes see their INR readings shift enough to demand dose recalibration. Possible gut flora changes? Enzyme tweaking? We can speculate, but what’s certain is that change means more frequent checks.
Put simply: warfarin is a diva. The smallest tweak—changing an antidiabetic agent, switching to a new meal plan, catching a stomach bug—can make her act up. The goal is to predict these flares before they hit, but no one’s a mind reader. That’s why everyday management matters so much, right down to the nitty gritty of patient education.

Spotting INR Fluctuations in Real Life: Common Pitfalls and Pearls
Every practicing clinician has that patient: the reliable, card-carrying diabetic who suddenly shows an INR of 7 or, worse yet, drops dangerously low right after a glucose med adjustment. It’s never just bad luck. There’s almost always a reason—if you dig deep enough. So, what are the danger zones? The most common triggers come down to new medications, dosage tweaks, lifestyle shifts, or missed meals due to hypoglycemia.
Real-world example: a 68-year-old who’s been on stable warfarin and gliclazide breaks her toe. She can’t manage her usual walks and starts eating less. Within ten days, her INR rockets, thanks to reduced vitamin K intake (blame those skipped leafy greens), and less plasma protein due to her altered nutritional state. If her warfarin dose isn’t held or cut down, she could be one fall away from a major bleed.
Another classic setup is a patient started on metformin after uncontrolled sugars—nothing fancy, just a new tablet. Two weeks later, the INR is up, even with no obvious dietary or illness-related changes. The culprit? A subtle boost in metformin’s impact on liver metabolism, unmasking a hidden interaction when layered on top of warfarin therapy. GPs who only check the INR monthly might miss the warning signs, but those running tight two-week checks catch the blip and adjust before trouble hits.
People don’t always follow a strict meal schedule, either—especially folks on insulin. Skipping meals can lead to hypoglycemia, which then leads to emergency foods, extra sugar, and sometimes even an ER visit. Each step along that path can jostle warfarin’s effect. Even just swapping out regular meals for meal replacements on the advice of a dietitian has tripped up patients before—unusual fiber or vitamin K content can nudge INR unpredictably.
How about over-the-counter supplements? Don’t ignore them. Some “natural” remedies popular among diabetics, like ginseng, turmeric, and cinnamon, can interact with warfarin directly or by affecting gut bacteria. There’s even been a small case series out of Perth’s Fiona Stanley Hospital showing INR spikes among warfarin users who started turmeric capsules.
So, where does this leave you in daily practice? It’s the small detail—a new med, a changed dosage, a new supplement—that should set off alarm bells and prompt quicker follow-up. Warfarin isn’t a set-and-forget drug. It needs someone watching its back, especially in people juggling multiple chronic conditions.
Curious about more specific scenarios? Check out this practical resource on warfarin and type 2 diabetes, which dives deeper into tricky cases and practical solutions straight from the clinic floor.
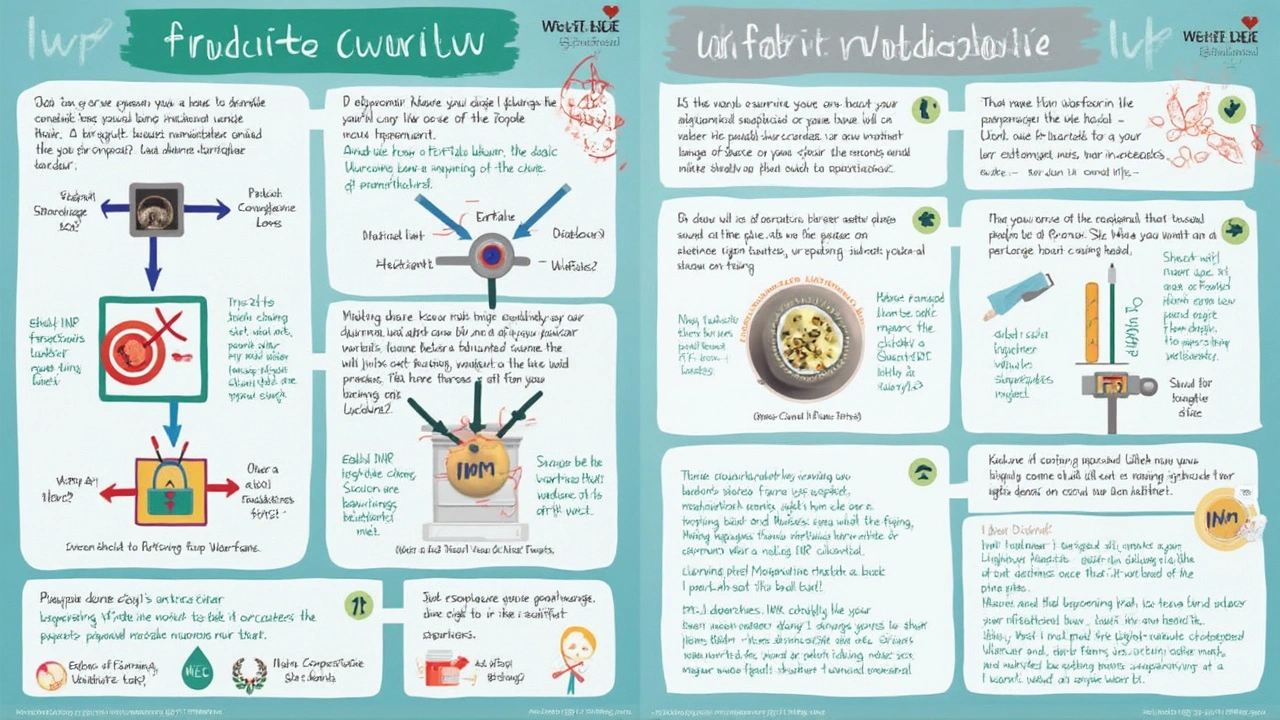
Pro Tips and Strategies to Tame the Warfarin–Diabetes Beast
So, what actually works when your diabetic patient’s INR starts to wobble? The old advice—“Monitor more often and adjust the dose slowly”—still rings true, but real-world tips make all the difference. Here’s how clinicians on the front lines keep things steady:
- Increase INR frequency whenever you change diabetic therapy. When switching from one antidiabetic agent to another, bump INR monitoring up to weekly for the first month. Use phone follow-ups or a simple telehealth check-in—it’s less hassle for the patient but lifesaving if a spike or drop appears.
- Keep a drug interaction checklist handy. The newest antidiabetic drugs aren’t always in the standard interaction software yet. Double-check for new updates or run through recent reviews. Don’t just trust your memory—especially in fast-changing med lists.
- Teach your patients about hidden interactions. Encourage them to write down every new pill, vitamin, or supplement. Get them to bring everything in for a “brown bag review,” at least twice a year. It helps you spot things like cinnamon capsules or vitamin K-rich greens that might slip through questioning.
- Watch for meal replacements and drastic diet changes. People with diabetes are told to eat better all the time, so you’ll see a lot of “I stopped bread and started this new shake” stories. This isn’t just about glucose—it’s about lost or suddenly increased vitamin K, protein shifts, and sometimes even altered drug absorption.
- Beware temporary illnesses. Gastro, fevers, sudden infections can mean skipped meals or vomiting. Those episodes flip not just glucose but warfarin metabolism, too. Warn patients: if they’re too ill to eat for more than a day, they should call for advice, not just ride it out.
- Automate reminders. People with multiple meds get confused, especially older adults juggling warfarin and diabetes scripts. Use pharmacy-packed blister packs or set up phone calendar reminders for INR check-ins. Gives everyone one less thing to forget.
If you want numbers to bring this issue home, try this: a 2023 audit out of Queensland’s chronic disease clinics showed that 18% of patients on combined warfarin and antidiabetic therapy had at least one INR result outside target range every two months. That’s nearly one in five—and most slips were tied to changes in diabetic drugs or unreported supplements.
| Antidiabetic Medication | Typical INR Effect | Special Comments |
|---|---|---|
| Metformin | Slight increase or stable | Monitor after dose changes |
| Sulfonylureas | Can increase INR | Watch for albumin competition |
| Insulin | Indirect INR changes | Think stress/hypoglycemia |
| SGLT2/DPP-4 inhibitors | Variable, sometimes increase | Still emerging evidence |
Staying ahead means building systems that spot emerging problems before they turn into emergencies. And when you need more help? Don’t hesitate to loop in a specialist pharmacist—they love getting into the weeds of drug-drug, drug-food, and even drug-herb interactions. Sometimes all it takes is one extra set of eyes to spot a problem brewing.
Managing warfarin and type 2 diabetes together isn’t a puzzle with one fixed solution. As new therapies and trends come online, those INR quirks will keep showing up in unexpected ways. The most successful clinicians are the ones who keep a healthy sense of skepticism—and never trust a “stable” INR unless they know exactly what else changed in their patient’s life that month. Stay curious, keep asking questions, and remember: every little detail matters when you’re trying to keep your patients safe.
