Vitamin D and Statin Tolerance Calculator
When a doctor prescribes a statin, the goal is simple: lower LDL cholesterol and cut the risk of heart attacks and strokes. Yet many patients stop the pill because of muscle aches, weakness, or unexplained fatigue. This phenomenon is known as statin‑associated muscle symptoms (Statin‑associated muscle symptoms, also called SAMS, affect up to 30% of new users). A hot debate has emerged around whether a patient’s vitamin D status might be the missing piece of the puzzle. Below we untangle the biology, the data, and the practical steps you can take today.
Statins 101: Why tolerance matters
Statins belong to the HMG‑CoA reductase inhibitor class, which blocks the liver’s production of cholesterol. Large meta‑analyses from the Cholesterol Treatment Trialists’ Collaboration show a 25‑35% reduction in major cardiovascular events for high‑risk patients. The catch? If a patient drops the drug, those benefits disappear. Studies estimate that 7‑29% of people on statins become statin‑intolerant, mainly because of muscle‑related side effects.
Vitamin D basics and deficiency thresholds
Vitamin D, measured as serum 25‑hydroxyvitamin D (25‑OH‑D), is a fat‑soluble vitamin that supports calcium homeostasis and muscle function. Clinical guidelines typically define deficiency as < 20 ng/mL, insufficiency as 20‑30 ng/mL, and sufficiency as >30 ng/mL. The 2017 study from PMC5644425 highlighted a striking split: patients with baseline 25‑OH‑D ≤20 ng/mL achieved a 90% statin‑tolerance rate after supplementation, versus only 33% for those above that threshold.
How low vitamin D could worsen muscle pain
The link isn’t just statistical; there are several plausible mechanisms. Vitamin D receptors sit on skeletal muscle fibers, and deficiency can lead to impaired calcium handling, reduced protein synthesis, and outright myopathy. In parallel, many statins are metabolized by cytochrome P450 enzymes (especially CYP3A4). Low vitamin D status may down‑regulate these enzymes, potentially increasing the plasma concentration of CYP‑metabolized statins and raising the risk of toxicity. Some investigators have even suggested that statins themselves modestly raise vitamin D levels, creating a feedback loop that varies by statin type.
Observational evidence: promising but noisy
Early case series and retrospective reviews painted a hopeful picture. Ahmed et al. (2009) reported that 92% of vitamin‑D‑deficient patients saw complete resolution of statin‑induced myalgia after supplementing to >30 ng/mL. Bell’s 2010 case series echoed this, with 4 of 6 patients improving. The 2015 PMC4525395 letter added that 53% of statin‑intolerant patients could stay on some statin after raising vitamin D above 30 ng/mL (average follow‑up 8.5 months).
Key take‑aways from the observational world:
- Most studies focus on patients already flagged as intolerant.
- Vitamin D repletion targets range from >30 ng/mL to >40 ng/mL.
- Pravastatin and rosuvastatin appear most tolerated after correction.
- Study designs are often uncontrolled, making it hard to separate placebo effect from true benefit.
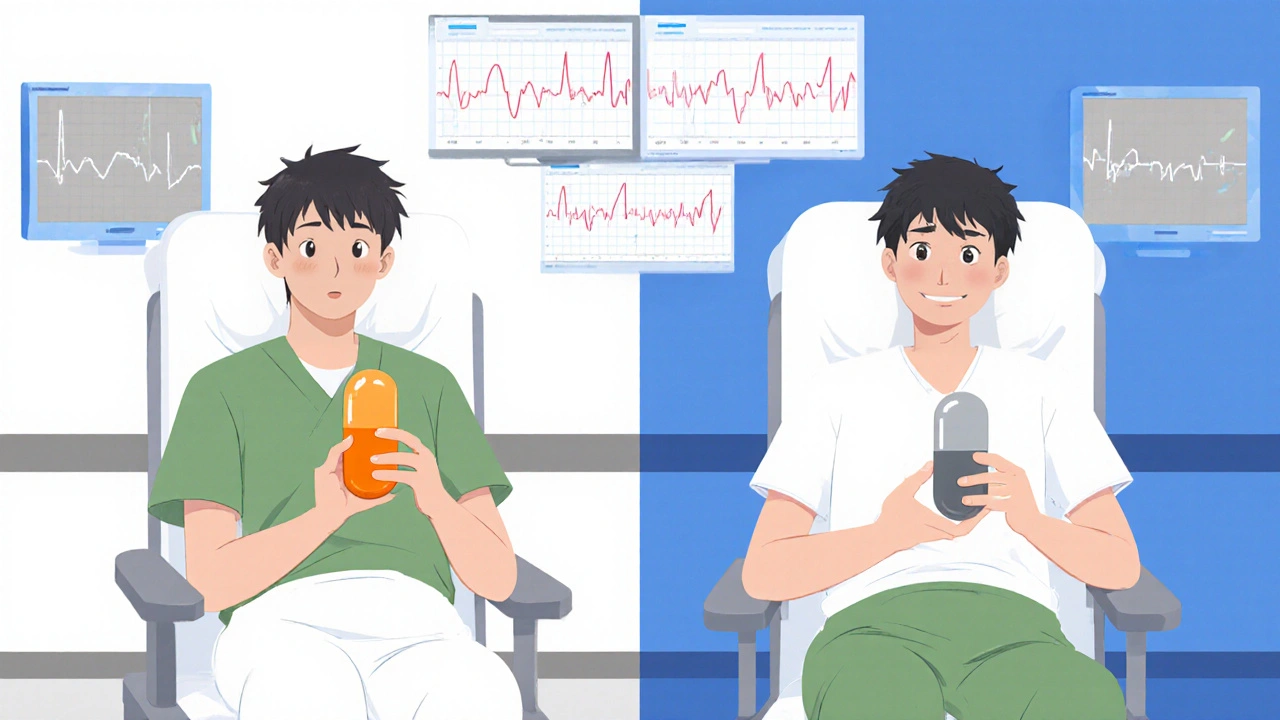
Randomized controlled trials: the reality check
The 2022 JAMA Cardiology sub‑analysis of the VITAL trial (2798958) is the first large‑scale RCT that directly tested the hypothesis. Over 2,000 participants starting statins were randomized to vitamin D3 2,000 IU daily or placebo. Results were blunt:
- Muscle symptoms occurred in 31% of both groups.
- Statin discontinuation rates were identical (13%).
- No subgroup (including those with baseline 25‑OH‑D <20 ng/mL) showed a meaningful advantage.
Why the gap?
- RCTs control for placebo effect, which can be substantial in subjective outcomes.
- Observational studies may capture patients with severe deficiency who truly benefit, a signal diluted in a broader trial.
- Differences in dosing (2,000 IU vs higher loading doses) and duration may matter.
Practical guide for clinicians and patients
Even with mixed data, many providers still measure vitamin D when faced with statin intolerance. Here’s a step‑by‑step approach you can use:
- Order a serum 25‑OH‑D test.
- If < 20 ng/mL, start vitamin D3 2,000-4,000 IU daily; aim for >30 ng/mL within 8‑12 weeks.
- Re‑challenge the original statin at the same dose; monitor for muscle pain.
- If symptoms recur, consider switching to a hydrophilic statin (pravastatin or rosuvastatin) that relies less on CYP3A4.
- Document tolerance and lipid panels; adjust dose only if LDL remains above target.
For patients with mild insufficiency (20‑30 ng/mL) who are already on a statin without symptoms, routine supplementation solely for tolerance is not evidence‑based according to the JAMA trial.
Side‑by‑side comparison of the evidence
| Study Type | Sample Size | Vitamin D Target | Statin Tolerance Outcome | Key Limitation |
|---|---|---|---|---|
| Observational (e.g., Ahmed 2009, Bell 2010) | 30-60 patients | >30 ng/mL after repletion | 70‑90% reported symptom resolution | No control group; placebo effect possible |
| Observational (PMC4525395, 2015) | 34 statin‑intolerant patients | >30 ng/mL | 53% remained on a statin ≥4 months | Retrospective, small cohort |
| Randomized Controlled (JAMA 2022, VITAL sub‑study) | 2,083 participants | 2,000 IU daily (no target level) | No difference in muscle symptoms or discontinuation | Broad population; may miss severe‑deficiency subgroup |
Bottom line for you
If you’re battling muscle aches on a statin, ask your doctor to check your 25‑hydroxyvitamin D. For those with a clear deficiency (<20 ng/mL), a short course of vitamin D3 supplementation often improves tolerance and lets you stay on a life‑saving statin. If your levels are already adequate, the current high‑quality evidence suggests that routine vitamin D won’t stop SAMS. In those cases, focus on statin type, dose spacing, or alternative lipid‑lowering strategies.
Frequently Asked Questions
Can vitamin D deficiency cause statin muscle pain?
Low 25‑OH‑D can weaken muscles and may amplify statin toxicity, especially for drugs cleared by CYP3A4. Observational data show improvement after repletion, but causality isn’t proven.
What vitamin D level should I aim for before restarting a statin?
Most clinicians target >30 ng/mL; the 2017 study found the biggest tolerance boost when baseline was ≤20 ng/mL and therapy raised the level above that cut‑off.
Which statin is safest after vitamin D correction?
Pravastatin and rosuvastatin have the lowest reliance on CYP3A4 and were most often tolerated in small re‑challenge trials.
Does taking vitamin D guarantee I won’t feel muscle aches?
No. The large JAMA RCT showed no overall benefit. Only a subset of patients with severe deficiency may see relief.
How long should I stay on vitamin D before re‑testing?
Eight to twelve weeks of 2,000-4,000 IU daily is enough for most adults to reach a stable serum level.
