Lamotrigine-Valproate Dosing Calculator
Safe Lamotrigine Dosing Calculator
Determine the appropriate starting dose and titration schedule when combining lamotrigine with valproate to minimize rash risk.
Rash Risk Assessment
Based on current dosing:
Low risk of serious rash when following proper dosing
When doctors prescribe lamotrigine and valproate together, they’re not just adding two medications-they’re mixing a high-risk combination that can trigger a dangerous skin reaction if not handled correctly. This isn’t theoretical. In the early 1990s, hospitals saw a spike in severe rashes, some turning into life-threatening conditions like Stevens-Johnson syndrome, all because the dosing wasn’t adjusted. Today, we know exactly why-and how to prevent it.
Why This Combination Is Risky
Valproate doesn’t just sit beside lamotrigine; it actively interferes with how the body processes it. Specifically, valproate blocks the liver enzyme that breaks down lamotrigine, slowing its clearance by nearly half. That means if you take both drugs without changing the lamotrigine dose, your blood levels of lamotrigine can double. And higher levels? That’s directly tied to a higher chance of rash. This isn’t a guess. Studies from the German registry of severe skin reactions show that before 1993, serious rashes from lamotrigine were common. After doctors started lowering the starting dose and slowing the titration, those cases dropped sharply. By 1999, severe rash rates had fallen from 1 in 890 exposures to less than 1 in 5,800. The fix wasn’t a new drug-it was a smarter dosing plan.What the Rash Looks Like-and When to Worry
Most rashes from lamotrigine start as a mild, red, flat patch on the face, chest, or arms. It might itch. It might spread. But here’s the catch: the first sign isn’t always the worst. In some cases, the rash evolves over days-even after stopping the drug. One 2023 case report described an 18-year-old who developed a full-body rash and swollen lymph nodes 12 days after starting the combo. Symptoms worsened for three more days after she stopped lamotrigine. That’s why you can’t wait to see if it "goes away on its own." Serious reactions include Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). These aren’t just bad rashes-they’re medical emergencies. SJS can cause blistering, peeling skin, and damage to the eyes and mouth. TEN is even worse, with over 30% of the skin detaching. Mortality rates for TEN can hit 35%. While these are rare now, they’re still possible-and they almost always happen in the first 8 weeks of treatment.The Right Way to Start Lamotrigine With Valproate
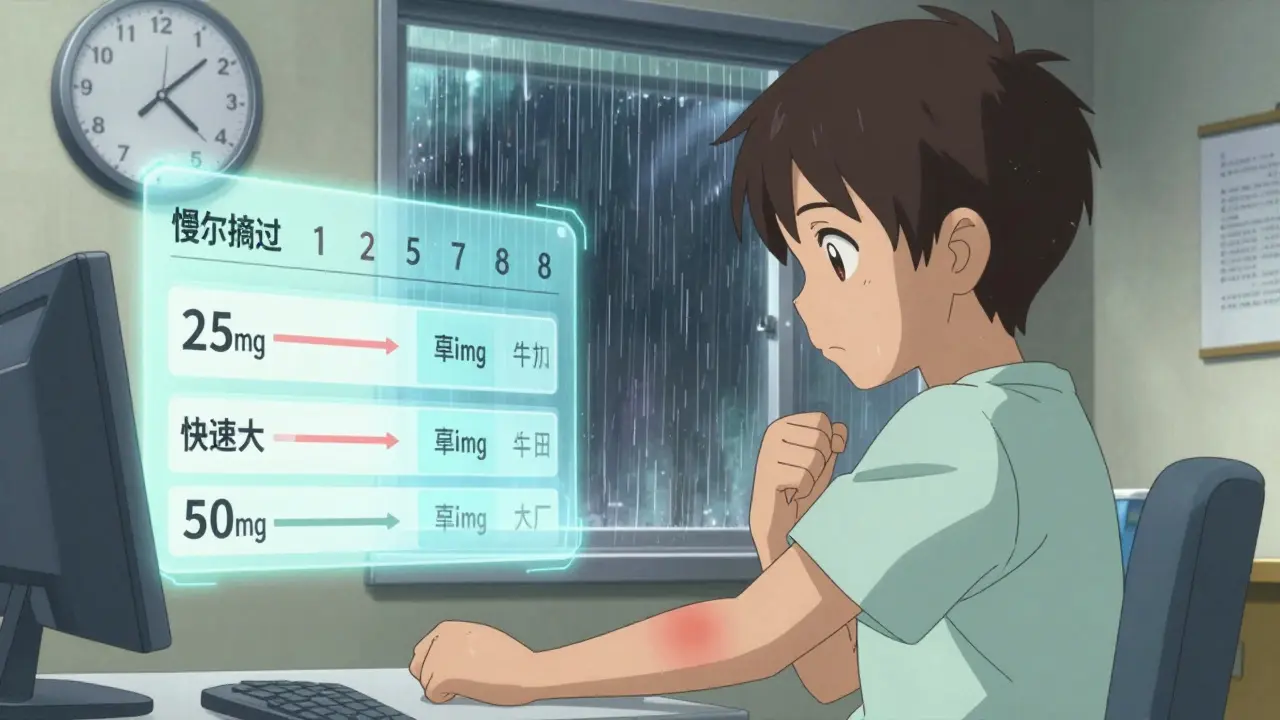
If you’re already taking valproate and your doctor wants to add lamotrigine, the starting dose must be cut in half-and then moved even slower.- Standard start (without valproate): 25 mg daily
- With valproate: 25 mg every other day (so, 12.5 mg per day on average)
- Weeks 1-2: 25 mg every other day
- Weeks 3-4: 25 mg daily
- Weeks 5-6: 50 mg daily
- Weeks 7-8: 75 mg daily
- Then increase by 50 mg every 2-4 weeks, depending on tolerance
What About Kids and Teens?
Some studies suggest children may have lower rash rates than adults, but that doesn’t mean they’re safe. In fact, the FDA issued a black box warning for lamotrigine in pediatric patients specifically because of the higher risk when combined with valproate. One 2025 study of 80 children and teens on both drugs found only two rashes-but those patients were closely monitored. Many doctors now start even lower: 12.5 mg every other day for kids under 18 on valproate. The key isn’t age-it’s caution. Even if a child has been on lamotrigine before without issues, adding valproate resets the risk. Always restart at the lowest dose.What Else Increases Risk?
It’s not just the combo. Other factors matter too:- Previous rash from any antiepileptic drug: If you’ve had a rash from carbamazepine, phenytoin, or even gabapentin, your risk jumps 3 times higher.
- Starting dose too high: Jumping to 50 mg or 100 mg right away is dangerous.
- Stopping valproate suddenly: If you stop valproate while still on lamotrigine, lamotrigine levels will suddenly rise-risking a rash even if you’ve been stable for months.

What to Do If a Rash Appears
If you notice any new skin changes-redness, bumps, blisters, peeling, or even just unusual itching-stop lamotrigine immediately. Don’t wait. Don’t call your doctor tomorrow. Stop it now. Then, contact your prescriber right away. Do not restart lamotrigine unless they say it’s safe. Even mild rashes can progress. In the cases where patients were treated early, symptoms cleared within days with antihistamines or short-term steroids. But if you wait, you could end up in the hospital.Why This Matters Beyond the Skin
Lamotrigine and valproate are powerful tools. Lamotrigine helps with bipolar depression and seizure control. Valproate works for seizures, migraines, and mood swings. Together, they can stabilize people who haven’t responded to anything else. But their interaction is one of the most well-documented-and preventable-drug risks in psychiatry and neurology. The good news? When dosed properly, the serious rash risk is now below 0.1%. That’s less than 1 in 1,000. That’s not zero-but it’s manageable. The difference between safety and danger is a simple dosing schedule. No new drugs. No expensive tests. Just patience and precision.Final Takeaway
You don’t need to avoid this combo. But you do need to respect it. The risk isn’t in the drugs-it’s in how they’re introduced. Follow the slow titration. Watch for skin changes. Stop at the first sign of rash. And never, ever start lamotrigine at a normal dose if you’re on valproate. That’s the only rule that matters.Can I take lamotrigine and valproate together safely?
Yes, but only if the lamotrigine dose is started very low and increased slowly. Starting lamotrigine at 25 mg every other day (instead of daily) and increasing by 25 mg every two weeks reduces the risk of serious rash to under 0.1%. Never start at the standard dose if you’re already on valproate.
How long does the rash risk last after starting lamotrigine?
Most rashes appear within the first 8 weeks of starting lamotrigine, but cases have been reported up to 12 weeks after starting-or even after stopping the drug. The risk is highest during the titration phase, but vigilance is needed for at least two months.
What if I’ve had a rash from another seizure medication before?
If you’ve had a rash from any antiepileptic drug-even carbamazepine or phenytoin-your risk of developing a rash from lamotrigine is three times higher. Talk to your doctor before starting. You may need an even slower titration or alternative treatment.
Does stopping valproate increase my lamotrigine rash risk?
Yes. If you stop valproate while still taking lamotrigine, your body will suddenly clear lamotrigine faster, causing levels to drop. But if you restart valproate later, lamotrigine levels will spike again-triggering a rash even if you’ve been stable for months. Always adjust lamotrigine when valproate is added or removed.
Are children at higher risk than adults?
The FDA warns that children are at higher risk for serious skin reactions when lamotrigine is combined with valproate. Some studies show lower rash rates in kids, but that’s likely because they’re monitored more closely. Most experts now recommend starting at 12.5 mg every other day for children and teens on valproate.
Can I restart lamotrigine after a mild rash?
Never restart lamotrigine after any rash without explicit approval from your doctor. Even a mild rash can be a warning sign for a life-threatening reaction if the drug is restarted. If you do restart, it must be under strict supervision with an extremely slow re-titration-and only if the rash was truly mild and resolved completely.
Is there a blood test to check if I’m at risk?
No. There are no validated genetic or blood tests to predict lamotrigine rash risk. The only reliable method is following the correct dosing schedule and watching for early skin changes. Blood levels of lamotrigine can be checked, but they’re not used to predict rash-they’re used to guide dosing after the fact.
What are the alternatives if I can’t take this combo?
For epilepsy, alternatives include levetiracetam, lacosamide, or clobazam. For bipolar disorder, lithium, quetiapine, or carbamazepine may be options-though carbamazepine also carries a rash risk. The choice depends on your diagnosis, past responses, and other health conditions. Always discuss alternatives with your prescriber before making changes.