Ulcerative Colitis: What You Need to Know
Ulcerative colitis (UC) is an inflammatory bowel disease that mainly affects the lining of the colon and rectum. It can show up at any age, but many people notice it in their 20s or 30s. The condition makes the gut wall swell, causing pain, urgency and blood in the stool. While there’s no cure yet, most folks can keep symptoms under control with the right mix of medicine, diet and lifestyle tweaks.
Common Signs and Symptoms
Typical UC flare‑ups start with cramping lower‑abdominal pain that gets worse after meals. You’ll likely feel the urge to go to the bathroom several times a day, and the stools often contain mucus or bright red blood. Weight loss, fatigue and a low‑grade fever are also common when the inflammation is active.
If you notice any of these signs lasting more than a week, especially blood in the stool, it’s a good idea to see a doctor. A simple colonoscopy or flexible sigmoidoscopy can confirm the diagnosis and show how far the disease has spread.
Managing Flare‑ups: Treatment and Lifestyle Tips
Doctors usually start with anti‑inflammatory drugs such as mesalamine (5‑ASA) to calm the gut lining. When symptoms are moderate to severe, steroids or immunosuppressants like azathioprine may be added. Biologic therapies (e.g., infliximab) are an option for people who don’t respond to the first‑line meds.
Medication works best when you pair it with a gut‑friendly diet. Many UC patients find relief by avoiding high‑fat, spicy or heavily processed foods. Instead, choose low‑residue meals like boiled chicken, white rice, peeled potatoes and ripe bananas during a flare. Adding a probiotic yogurt or kefir can help restore healthy bacteria, but keep an eye on dairy if it triggers symptoms.
Staying hydrated is crucial—drink plenty of water, herbal teas or clear broths. Dehydration can worsen cramps and make stools harder to pass. Small, frequent meals tend to be gentler on the colon than large plates.
Stress management can also affect UC. Simple practices like short walks, breathing exercises, or a few minutes of meditation each day often lower the frequency of flare‑ups. If you’re juggling work or school, try to schedule regular breaks and keep a symptom diary; it helps you and your doctor spot patterns.
Regular check‑ups are a must. Your doctor will monitor blood work, colon health and any medication side effects. Keeping up with vaccinations, especially flu and COVID‑19 shots, reduces infection risk while you’re on immunosuppressants.
In short, ulcerative colitis doesn’t have to control your life. Knowing the warning signs, sticking to a tailored treatment plan, and making a few everyday adjustments can keep you feeling steady and active. If you’re unsure where to start, talk to your healthcare provider about a step‑by‑step plan that fits your routine.
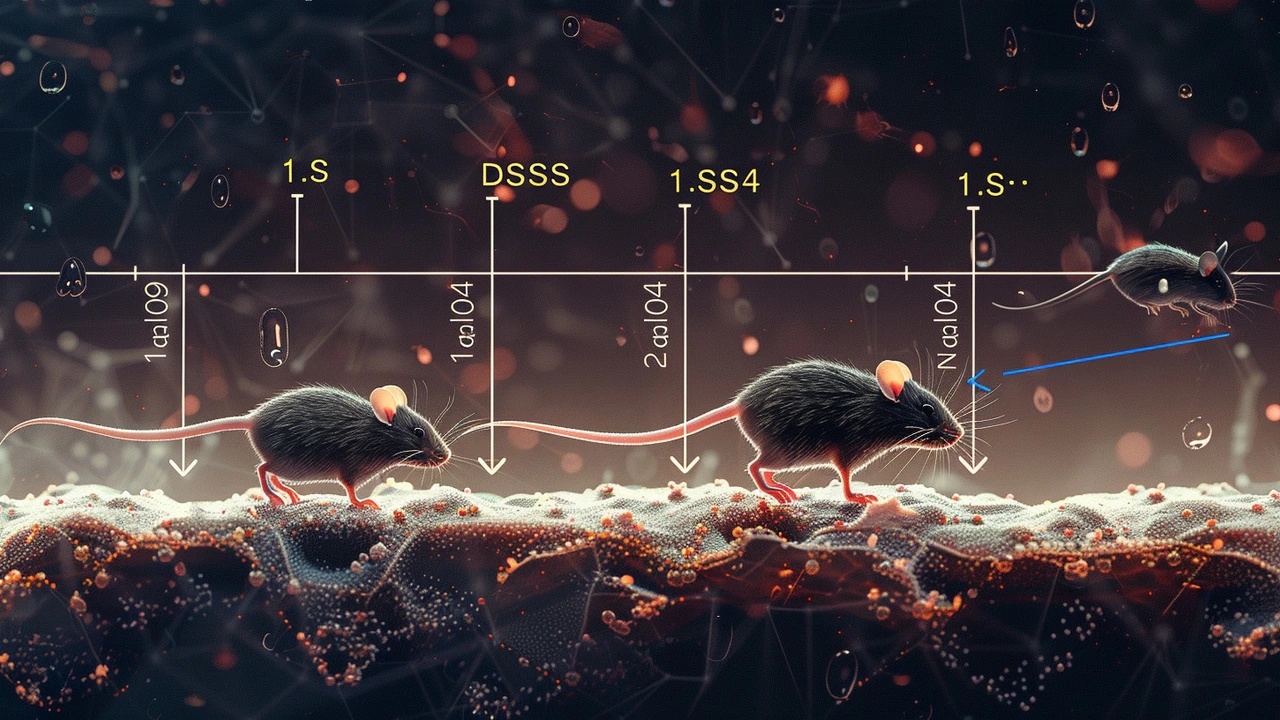
Mebendazole: A Breakthrough in Ulcerative Colitis Treatment Through Suppression of Inflammation and Stress
Recent research reveals Mebendazole, a known anthelmintic drug, effectively reduces inflammation and oxidative stress in mice with ulcerative colitis. Comparison with standard treatments shows promising results, sparking discussions on its potential repurposing for human UC therapy. Further studies are anticipated to explore its efficacy and safety in humans.
Learn more...