Statin Myopathy Risk Calculator
How likely are you to experience muscle pain from statins?
This calculator estimates your risk based on factors identified in medical research. Results are for informational purposes only and not a substitute for professional medical advice.
Your Risk Factors
Protective Factors
Your Risk Assessment
For millions of Americans taking statins to lower cholesterol, muscle pain isn't just an inconvenience-it's a dealbreaker. About 1 in 3 people on statins report muscle discomfort, cramps, or weakness. For some, it's mild and temporary. For others, it’s severe enough to stop the medication entirely. This isn't just about discomfort. It’s about a real, biologically driven condition called statin-associated muscle symptoms (SAMS), and in its worst form, statin-induced myopathy.
What Exactly Is Statin-Induced Myopathy?
Statin myopathy isn’t just sore muscles after a workout. It’s a drug-induced muscle disorder caused by how statins interfere with muscle cell function at the molecular level. The most serious form involves elevated creatine kinase (CK) levels-more than 10 times the normal range-along with muscle weakness and pain. While only 0.1% to 0.5% of users develop this severe version, up to 30% experience milder muscle symptoms that still impact daily life.Symptoms usually show up within the first six months of starting a statin. People describe it as deep, persistent aching-not sharp pain, but a heavy, tired feeling in the thighs, shoulders, or back. Some notice they can’t climb stairs like they used to. Others wake up stiff and sore, even without physical activity. The good news? In 80% of cases, symptoms fade within 1 to 4 weeks after stopping the statin.
The Science Behind the Pain: Three Key Mechanisms
Researchers now understand that statin myopathy isn’t caused by one single problem-it’s a cascade of three interconnected biological disruptions.1. Calcium Leaks in Muscle Cells
Statins cause a protein called FKBP12 to detach from the ryanodine receptor (RyR1), a calcium channel in muscle cells. When FKBP12 isn’t holding it in place, the channel leaks calcium uncontrollably. Studies show this increases calcium sparks-tiny bursts of calcium release-by 2.3 times in human muscle tissue. These leaks trigger enzymes that break down muscle fibers and activate cell death pathways. What’s striking is that this only happens in skeletal muscle, not the heart. That’s why your heart keeps beating fine while your legs feel like lead.2. Depletion of Essential Molecules
Statins block HMG-CoA reductase, the enzyme that makes cholesterol. But that same enzyme also produces isoprenoids like farnesyl pyrophosphate and geranylgeranyl pyrophosphate. These molecules help attach proteins to cell membranes so they can function properly. When statins cut their production by 60-80%, key signaling proteins in muscle cells stop working. This disrupts how muscles contract, repair, and respond to stress.3. CoQ10 Drop and Energy Crisis
Coenzyme Q10 (CoQ10) is critical for mitochondrial energy production. Statins reduce muscle CoQ10 levels by about 40% within four weeks. Without enough CoQ10, muscle cells struggle to make ATP-their main energy source. This leads to fatigue and increased oxidative stress. Studies show reactive oxygen species (ROS) rise by 35% in statin-treated muscle, damaging cell structures over time.The Rare but Serious Autoimmune Form
A small subset of patients-about 5-10% of those with persistent myopathy-develop an autoimmune version. Their immune system starts making antibodies against HMG-CoA reductase, the very enzyme statins target. This is called anti-HMGCR myositis. About 60% of these patients had taken statins before symptoms appeared. It’s rare-only 0.02% of statin users-but it’s serious. Muscle weakness can become severe, and standard statin cessation doesn’t help. These patients often need immunosuppressants like methotrexate and prednisone. Without treatment, the condition can progress to permanent muscle damage.
Why Some People Are More at Risk
Not everyone on statins gets muscle problems. Certain factors increase risk:- Age over 75
- Low body weight or frailty
- Chronic kidney or liver disease
- Taking other drugs that interact with statins-like fibrates, cyclosporine, or certain antibiotics
- Genetic variants in drug metabolism genes (SLCO1B1)
- High-dose statins (especially atorvastatin 80 mg or rosuvastatin 20 mg)
- Sedentary lifestyle
Interestingly, people who exercise regularly are less likely to develop symptoms. A 2021 Mayo Clinic study found that those who did 150 minutes of moderate exercise per week reported 41% fewer muscle issues than sedentary users. Exercise appears to help stabilize the RyR1 channel and reduce calcium leaks.
What to Do If You Have Muscle Pain
If you start feeling unexplained muscle aches after beginning a statin, don’t ignore it. Don’t assume it’s just aging or overtraining. Here’s what to do:- Track your symptoms: Note when they started, where they hurt, and how bad they are on a scale of 1-10.
- Don’t stop the statin on your own: Stopping abruptly can raise your cholesterol and increase heart risk. Talk to your doctor first.
- Get a CK blood test: This measures muscle damage. Levels above 5 times the upper limit suggest statin myopathy.
- Try a washout period: Your doctor may ask you to stop the statin for 4 weeks. If symptoms improve, it’s likely related.
Managing Statin Myopathy: Proven Strategies
Once confirmed, there are several evidence-backed ways to manage it:Switch statins
Not all statins are equal. Pravastatin and fluvastatin are less likely to cause muscle issues because they’re cleared differently by the liver. About 40% of people who couldn’t tolerate one statin tolerate another.Lower the dose
Many people respond well to a lower dose. A 2022 study showed 65% of patients could stay on a reduced dose without symptoms returning. Sometimes, taking the statin every other day works too.Try CoQ10 supplements
A 2022 European study found that 200 mg of CoQ10 daily reduced muscle pain in 35% of patients. Some report feeling better within 2-4 weeks. While not a cure, it’s low-risk and worth trying.Move more
Moderate exercise-brisk walking, cycling, swimming-is one of the most effective tools. A 2023 clinical trial showed that 150 minutes per week of activity reduced calcium leaks and improved muscle symptoms by 52%. Exercise doesn’t make it worse-it helps.Switch to non-statin options
If muscle pain persists, alternatives exist:- Ezetimibe: Lowers LDL by about 30% with minimal muscle side effects.
- PCSK9 inhibitors (like evolocumab): Injectable drugs that cut LDL by 60%. Muscle-related side effects are only 3.7%-lower than placebo.
- Bempedoic acid: A newer oral drug that works in the liver, not muscles, with only 2.5% muscle pain rates.
The Future: New Statins and Targeted Therapies
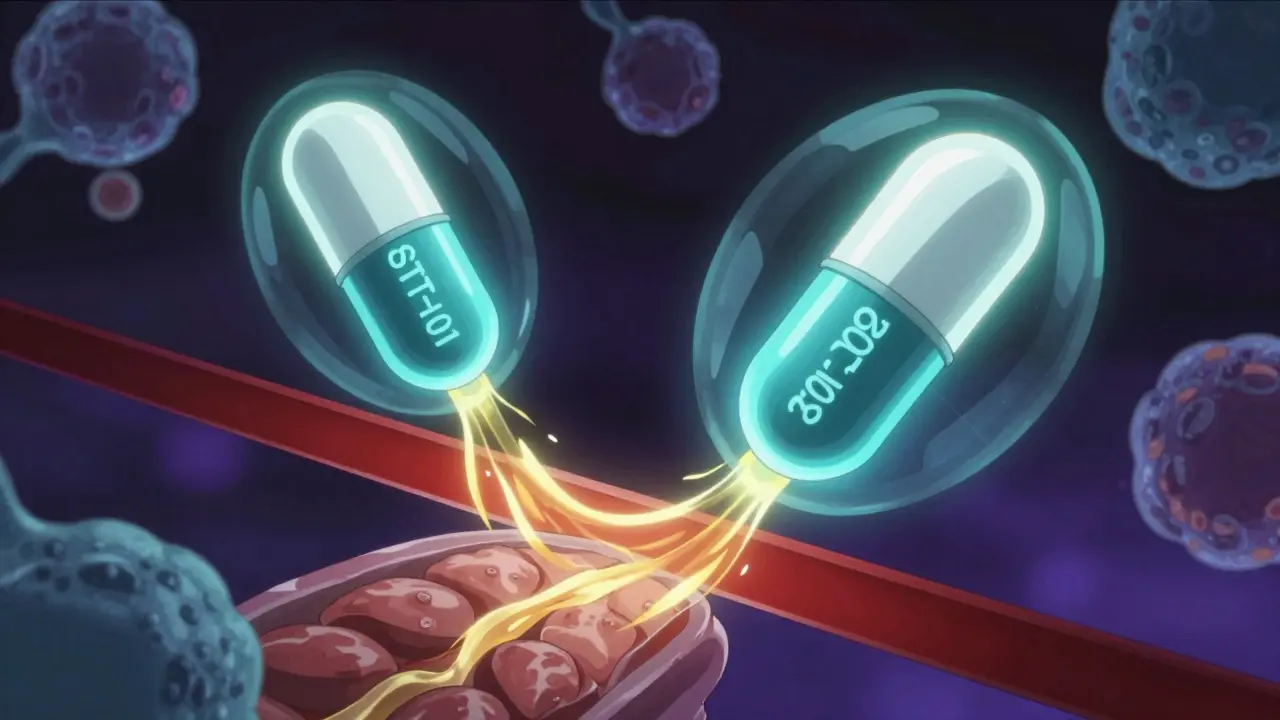
Researchers are developing smarter statins. Two new compounds-STT-101 and STT-202-are in early trials. They’re designed to stay in the liver and avoid muscle tissue entirely, reducing muscle penetration by 70% compared to atorvastatin.Another promising drug, S107, stabilizes the RyR1 calcium channel. In a 2023 phase II trial, it cut calcium leaks by 65% and reduced muscle symptoms by over half. It’s not available yet, but it points to a future where muscle pain from statins could be prevented, not just managed.
Combining CoQ10 with exercise has shown even better results: 80% symptom resolution in one 2024 study. That’s higher than either approach alone.
Why This Matters Beyond Muscle Pain
Many people stop statins because of muscle pain. But here’s the risk: a 2022 American Heart Association survey found that 31% of patients with muscle symptoms reduced their adherence, which raised their heart attack risk by 25% over five years.Statin therapy saves lives. For someone with heart disease or high cholesterol, the benefit outweighs the risk. The goal isn’t to avoid statins-it’s to find a way to take them safely.
Doctors are now trained to talk about muscle risks before prescribing. In 2023, 78% of cardiologists routinely discussed this with patients. That’s progress. But it’s up to you to speak up if something feels off.
Bottom Line: You Have Options
Muscle pain on statins isn’t a sign you’re weak or overdoing it. It’s a biological response-and it’s treatable. You don’t have to suffer through it. You don’t have to quit your medication either. Work with your doctor to test, adjust, or switch. Try CoQ10. Get moving. Explore alternatives. The science now gives you real tools to manage this-not just endure it.Statin myopathy is common, but it’s not inevitable. With the right approach, most people can stay on therapy without pain. And for those who can’t, there are safe, effective alternatives that protect the heart just as well.
Can statins cause permanent muscle damage?
In most cases, muscle damage from statins is reversible. Symptoms usually go away within weeks after stopping the drug. However, in the rare autoimmune form-anti-HMGCR myositis-muscle weakness can become severe and persistent without immunosuppressive treatment. Early diagnosis and therapy with drugs like prednisone and methotrexate can prevent long-term damage in these cases.
Does CoQ10 really help with statin muscle pain?
Yes, multiple clinical studies show CoQ10 supplementation (200 mg daily) reduces muscle pain in about one-third of patients. While it doesn’t work for everyone, it’s safe, inexpensive, and worth a 4-6 week trial. It helps restore mitochondrial energy production, which statins impair. Many patients report feeling less fatigued and less achy within a few weeks.
Should I stop my statin if I have muscle pain?
No, don’t stop on your own. Stopping statins without medical guidance can increase your risk of heart attack or stroke. Instead, contact your doctor. They may order a CK blood test, suggest a short washout period, or switch you to a different statin or non-statin therapy. Most cases can be managed without quitting statins entirely.
Can exercise make statin muscle pain worse?
No-exercise actually helps. A 2023 JUPITER trial subanalysis showed people who exercised 150 minutes per week had 32% lower creatine kinase levels and 41% fewer symptoms than sedentary users. Moderate activity like walking or cycling appears to stabilize calcium channels in muscle cells, reducing the leak that causes pain. Avoid extreme workouts, but don’t avoid movement.
Are newer statins safer for muscles?
Yes. Pravastatin and fluvastatin are less likely to cause muscle issues because they’re metabolized differently and don’t penetrate muscle tissue as much. Two experimental statins-STT-101 and STT-202-are currently in early trials and designed to stay in the liver, reducing muscle exposure by 70%. These could be game-changers for people who’ve had to quit statins due to muscle pain.
What’s the best alternative to statins if I can’t tolerate them?
Ezetimibe is a good first option-it lowers LDL by 20-30% with very low muscle side effects. For higher risk patients, PCSK9 inhibitors like evolocumab reduce LDL by 60% and have muscle adverse event rates lower than placebo. Bempedoic acid is another oral option that works in the liver and causes minimal muscle pain. These alternatives are proven to reduce heart attack and stroke risk, just like statins.
