When your lower back aches after standing too long, or your hamstrings feel tight no matter how much you stretch, it might not just be a bad posture or overworked muscles. For about 6% of adults, that persistent discomfort could be spondylolisthesis - a condition where one vertebra slips forward over the one below it. It’s not rare. It’s not always painful. But when it is, it can change how you move, sit, walk, and live.
What Exactly Is Spondylolisthesis?
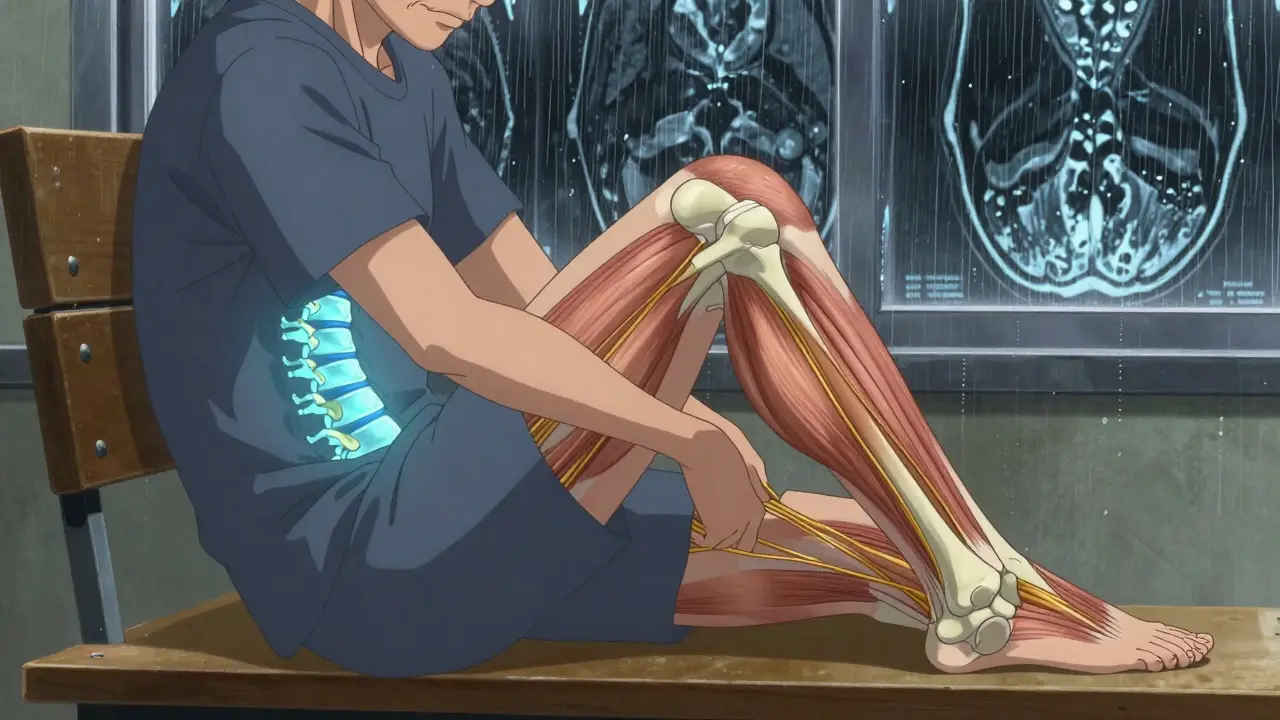
Spondylolisthesis comes from Greek: spondylo means vertebra, and olisthesis means slip. So, it’s literally a slipped vertebra. But it’s not like a bone sliding out of place like a dislocated shoulder. It’s a slow, progressive shift - usually in the lower spine, between the fifth lumbar vertebra (L5) and the first sacral bone (S1). This slippage doesn’t always cause symptoms. In fact, nearly half of people with it don’t even know they have it. But when it does, the pain can feel like a deep, dull ache in the lower back that radiates into the buttocks and thighs. It gets worse when you stand or walk, and eases when you sit or bend forward.Why Does It Happen? Five Different Causes
Not all spondylolisthesis is the same. The cause determines how it’s treated. There are five main types:- Degenerative: The most common type in adults over 50. It’s caused by years of wear and tear on the spinal joints and discs. Arthritis breaks down the cartilage, letting the vertebra slip. This accounts for about 65% of adult cases.
- Isthmic: Often starts in childhood or adolescence. A small stress fracture in the pars interarticularis - a thin bone bridge between spinal joints - weakens the structure. Gymnasts, football players, and weightlifters are at higher risk because their sports involve repeated backward bending of the spine.
- Dysplastic: A birth defect. The spinal joints are malformed from the start, making slippage more likely. This is rare but often shows up in kids under 6.
- Pathologic: Caused by diseases that weaken bone - like tumors, infections, or osteoporosis. The vertebra can’t hold its position.
- Traumatic: Results from a sudden injury - a fall, car crash, or hard impact - that fractures the vertebra.
How Bad Is It? The Meyerding Scale
Doctors grade the severity of slippage using the Meyerding Classification. It’s based on how far one vertebra has slipped over the one below it, measured as a percentage of the vertebral body’s width:- Grade I: 1% to 25% slippage - mild, often asymptomatic
- Grade II: 26% to 50% - moderate, may cause discomfort
- Grade III: 51% to 75% - severe, often with nerve symptoms
- Grade IV: 76% to 100% - very severe, high risk of nerve compression
- Grade V (Spondyloptosis): More than 100% - the vertebra has completely slipped off the one below
What Does It Feel Like? Symptoms Beyond Back Pain
The most obvious sign is lower back pain - but it’s not always the worst part. Many people notice:- Tight hamstrings (70% of symptomatic patients)
- Stiffness in the lower back
- Difficulty standing or walking for long periods
- Pain that shoots down one or both legs (sciatica)
- A noticeable swayback (increased lordosis) - or later, a rounded back (kyphosis)
How Is It Diagnosed?
It starts with a simple X-ray - standing lateral views are key. That’s because the slip often gets worse when you’re upright. If the X-ray shows slippage, the next step is usually an MRI. That tells doctors if nerves are being squeezed, if discs are worn down, or if there’s inflammation. A CT scan might follow if they need to see the bone structure in detail - especially if they suspect a stress fracture in the pars interarticularis. What they’re looking for isn’t just how far the bone has slipped, but how much damage has been done to the surrounding tissues. Research shows that the degree of disc degeneration correlates more strongly with age than with the slippage grade. That means two people with the same slip percentage might have very different levels of pain - one because of worn discs, the other because of muscle tightness. Treatment should match the cause, not just the X-ray.Non-Surgical Treatment: What Actually Works
Most people - up to 80% - never need surgery. The first line of defense is conservative care:- Activity modification: Avoid sports or movements that arch the back - like heavy lifting, gymnastics, or football. Switch to swimming or cycling.
- Physical therapy: Focuses on core strengthening (transverse abdominis, multifidus), hamstring stretching, and posture retraining. Studies show it takes 12 to 16 weeks of consistent therapy to see real improvement. Only about 65% of patients stick with it long enough.
- Medications: NSAIDs like ibuprofen or naproxen help reduce inflammation and pain. They don’t fix the slip, but they make daily life manageable.
- Epidural steroid injections: For those with nerve pain, these shots can reduce swelling around compressed nerves. They’re not a cure, but they can buy time for other treatments to work.
When Surgery Becomes Necessary
Surgery is considered when:- Conservative treatment has failed after 6 to 12 months
- Pain is severe and disabling
- There’s progressive nerve damage - leg weakness, loss of bladder control, or foot drop
- The slip is Grade III or higher
- Posterolateral fusion: Bone graft is placed along the back of the spine. The most common method - used in about 55% of cases. Success rate: 75-85% for Grade I-II, drops to 60-70% for Grade III-IV.
- Interbody fusion (PLIF/TLIF): The damaged disc is removed and replaced with a spacer filled with bone graft. This restores disc height and opens up space for nerves. Used in 35% of cases. Success rate: 85-92% across all grades.
- Minimally invasive fusion: Smaller incisions, less muscle damage. Used in about 10% of cases. Recovery is faster, but long-term data is still limited.

What Happens After Surgery?
Recovery isn’t quick. After fusion:- First 6-8 weeks: No lifting, twisting, or bending. You’ll wear a brace if needed.
- Months 2-6: Physical therapy focuses on gentle mobility and core control.
- By 12-18 months: Most patients reach full recovery.
New Options on the Horizon
The field is changing. In 2022, the FDA approved two new interbody devices designed specifically for spondylolisthesis. Early results show 89% fusion rates at six months - better than older models. Biologics like bone morphogenetic protein (BMP) and stem cell therapies are being tested. One 2023 trial found BMP-2 pushed fusion rates to 94% in high-risk patients, compared to 81% with traditional bone grafts. There’s also growing interest in motion-preserving alternatives - dynamic stabilization devices that allow limited movement instead of locking the spine completely. Early studies show 76% success at five years, compared to 88% for fusion. They’re not ready for everyone - mostly used for Grade I-II slips - but they offer hope for younger patients who want to keep more spine motion.What You Can Do Now
If you’re dealing with chronic lower back pain:- Don’t ignore it. See a doctor if it lasts more than 3-4 weeks.
- Stop activities that make it worse - especially those involving back extension.
- Start stretching your hamstrings daily. Tight hamstrings pull on the pelvis and worsen slippage.
- If you smoke, quit. Smokers have more than three times the risk of failed fusion.
- Manage your weight. A BMI over 30 increases surgical complications by 47%.
Can spondylolisthesis heal on its own?
No, the slipped vertebra won’t move back into place on its own. But the pain and symptoms often improve with conservative treatment - physical therapy, activity changes, and pain management. The goal isn’t to reverse the slip, but to stabilize the spine and reduce pressure on nerves. Many people live without symptoms once they adjust their movement patterns and strengthen supporting muscles.
Is spondylolisthesis the same as a herniated disc?
No. A herniated disc is when the soft cushion between vertebrae bulges or ruptures, pressing on nerves. Spondylolisthesis is when one bone slips forward over another. They can happen together - a slipped vertebra often causes disc degeneration - but they’re different conditions. An MRI can tell them apart.
Can I still exercise with spondylolisthesis?
Yes - but not all exercises are safe. Avoid activities that arch your back, like heavy weightlifting, gymnastics, or football. Safe options include swimming, walking, cycling, and yoga poses that focus on forward bending and core stability. A physical therapist can design a program that strengthens your spine without worsening the slip.
Does every case of spondylolisthesis need surgery?
No. Most people - around 80% - improve with non-surgical care. Surgery is only considered if pain is severe, conservative treatment has failed for 6-12 months, or there’s nerve damage like leg weakness or loss of bladder control. The degree of slippage alone doesn’t determine if you need surgery - symptoms do.
How long does it take to recover from spinal fusion?
Full recovery takes 12 to 18 months. The first 6-8 weeks involve rest and limited movement. Physical therapy starts around week 6 and continues for 3-6 months. Bone fusion takes time - it’s not just healing skin and muscle, but growing new bone between vertebrae. Most people return to light work by 3-4 months and full activity by 12-18 months.
What are the risks of spinal fusion surgery?
Risks include infection, nerve damage, blood clots, and failure of the bone to fuse (pseudoarthrosis). Smokers and people with high BMI have higher risks. About 12-15% of patients with severe slips need a second surgery, often because the spine above or below the fusion starts to break down over time. Success rates are high - 85-92% for interbody fusion - but it’s still major surgery with long-term implications.
