Hyponatremia Risk Assessment Tool
Medication Risk Assessment
This tool helps you understand your risk of severe hyponatremia (sodium below 120 mmol/L) from common medications. Based on your inputs, you'll receive personalized prevention recommendations.
Your Risk Assessment
Prevention Recommendations
- Get a baseline sodium test before starting any high-risk medication
- Ask for a sodium test within 7 days of starting a new medication
- Monitor for early symptoms like nausea, headache, and fatigue
- If symptoms develop, get tested immediately (do not wait)
- Discuss with your doctor about risk-reducing alternatives
- If you're over 65, ask for more frequent monitoring (every 3-5 days)
When your sodium levels drop too low, your brain starts to swell. It’s not a metaphor. It’s physics. And when that happens because of a medication you were told was safe, the consequences can be sudden, terrifying, and sometimes deadly. Severe hyponatremia - serum sodium below 120 mmol/L - doesn’t always come with warning signs. One day you feel a little off, the next you’re having seizures. This isn’t rare. It’s happening in hospitals, nursing homes, and even in the homes of people who thought they were just managing depression or high blood pressure.
What Exactly Is Medication-Induced Hyponatremia?
Hyponatremia means your blood has too little sodium - below 135 mmol/L. Severe cases fall under 120 mmol/L. Sodium isn’t just table salt. It’s critical for nerve and muscle function, fluid balance, and brain cell stability. When sodium drops too fast, water rushes into brain cells to balance the concentration. The brain swells. Pressure builds. Confusion, seizures, coma - these aren’t random symptoms. They’re direct results of brain swelling.
Medications are responsible for 17-20% of all severe hyponatremia cases in hospitals. That’s one in five. And it’s not just one drug. It’s a whole group. Diuretics like hydrochlorothiazide, antidepressants like sertraline and citalopram, epilepsy drugs like carbamazepine, and even common painkillers like ibuprofen can trigger it. The mechanism? Most often, it’s SIADH - the syndrome of inappropriate antidiuretic hormone secretion. Your body starts holding onto water like it’s running out, diluting your sodium without you realizing it.
The Red Flags: Confusion, Seizures, and Why They’re Missed
Early signs are easy to ignore. Nausea. Headache. Fatigue. People chalk it up to the flu, stress, or aging. But when sodium drops below 125 mmol/L, 45% of patients start showing neurological symptoms. Below 115 mmol/L, seizures become likely. In one documented case, a 72-year-old woman developed a grand mal seizure just 10 days after starting sertraline. Her sodium had dropped 0.8 mmol/L per day - fast enough to kill brain cells.
Doctors miss this. A lot. Studies show 15-20% of medication-induced hyponatremia cases are misdiagnosed as psychiatric conditions. Anxiety. Dementia. Depression. Why? Because the symptoms look the same. Memory lapses. Mood swings. Disorientation. But here’s the difference: these symptoms appear suddenly after starting a new drug, usually within one to four weeks. They don’t slowly creep in over months like dementia. And they reverse - often dramatically - when the drug is stopped and sodium is corrected properly.
On patient forums, the same story repeats: “My doctor didn’t warn me.” “I thought it was just side effects.” “I was hospitalized for five days because of low sodium from citalopram.” One in four negative reviews for SSRIs on Drugs.com mention hyponatremia. The warning labels exist. But they’re buried in fine print. And most patients never hear about it.
Who’s at Highest Risk?
This isn’t random. Certain people are far more vulnerable. Women make up 57% of severe cases. People over 65 account for 61%. Why? Older bodies process drugs slower. Hormonal changes in women affect fluid balance. And many are on multiple medications - a perfect storm.
Take someone on a diuretic for high blood pressure, then prescribed an SSRI for anxiety. That combination increases risk by 3.5 times compared to either drug alone. Carbamazepine carries the highest individual risk - 5.3 times more likely to cause hyponatremia than non-users. Even MDMA, an illicit drug, is linked to fatal hyponatremia because it triggers massive water retention.
And here’s the cruel twist: the people most at risk are often the ones least likely to report early symptoms. Elderly patients may not notice mild confusion. They might just say, “I’m tired.” Or they’re in a care facility where staff assume changes in behavior are “just part of aging.”
How Is It Diagnosed and Treated?
If you suspect hyponatremia, the first step is a simple blood test: serum sodium level. But diagnosis isn’t just about the number. It’s about timing. Did symptoms start after beginning a new medication? Are there signs of fluid overload - no swelling in legs, normal blood pressure? That points to SIADH, not heart or kidney failure.
Emergency treatment is urgent. But here’s the catch: correcting sodium too fast can be just as dangerous. If you raise it more than 8 mmol/L in 24 hours, you risk osmotic demyelination syndrome - a condition where brain cells lose their protective coating, leading to permanent paralysis, locked-in syndrome, or death. That’s why correction must be slow, controlled, and monitored in a hospital.
Standard care includes fluid restriction and stopping the offending drug. In severe cases, doctors may use hypertonic saline (3% sodium solution) to gently raise sodium levels. Newer drugs like tolvaptan (Samsca), approved in late 2023, help the body excrete excess water without losing sodium. Clinical trials show it cuts correction time by 34% compared to older methods.
Prevention: What You Can Do
The best treatment is avoiding it in the first place. Here’s how:
- Ask for a baseline sodium test before starting any high-risk medication - especially SSRIs, diuretics, or antiepileptics.
- Get tested again within 7 days of starting the drug. The American Geriatrics Society recommends repeat testing every 3-5 days for the first month in people over 65.
- Know your symptoms. If you develop unexplained nausea, headache, confusion, or muscle cramps after starting a new pill, don’t wait. Get your sodium checked.
- Ask your pharmacist. Pharmacists are trained to spot dangerous drug interactions. One patient credited their pharmacist with catching a potential interaction between oxcarbazepine and a diuretic - saving them from the same fate their sister suffered.
- Don’t assume it’s “just side effects”. If symptoms are new, worsening, or unusual, push for bloodwork. Your life could depend on it.
Why Is This Still Happening?
It’s not just patient ignorance. It’s systemic. Only 63% of prescribers follow recommended sodium monitoring guidelines. Academic hospitals do better - 82% screen high-risk patients. Community clinics? Only 47%. The FDA updated warnings in 2022 for 27 high-risk drugs. But there’s no enforcement. No penalty for skipping a test.
Dr. Robert Stern put it bluntly in JAMA Internal Medicine: “Why aren’t we mandating sodium checks in the first 30 days of high-risk drug therapy? We check liver enzymes for statins. We check kidney function for NSAIDs. Why not sodium?”
And the numbers don’t lie. Hyponatremia-related hospitalizations cost the U.S. $473 million a year - almost half a billion dollars - mostly from preventable medication cases. And it’s rising. SSRI prescriptions are up nearly 20% since 2018. The aging population is growing. More drugs. More seniors. More risk.
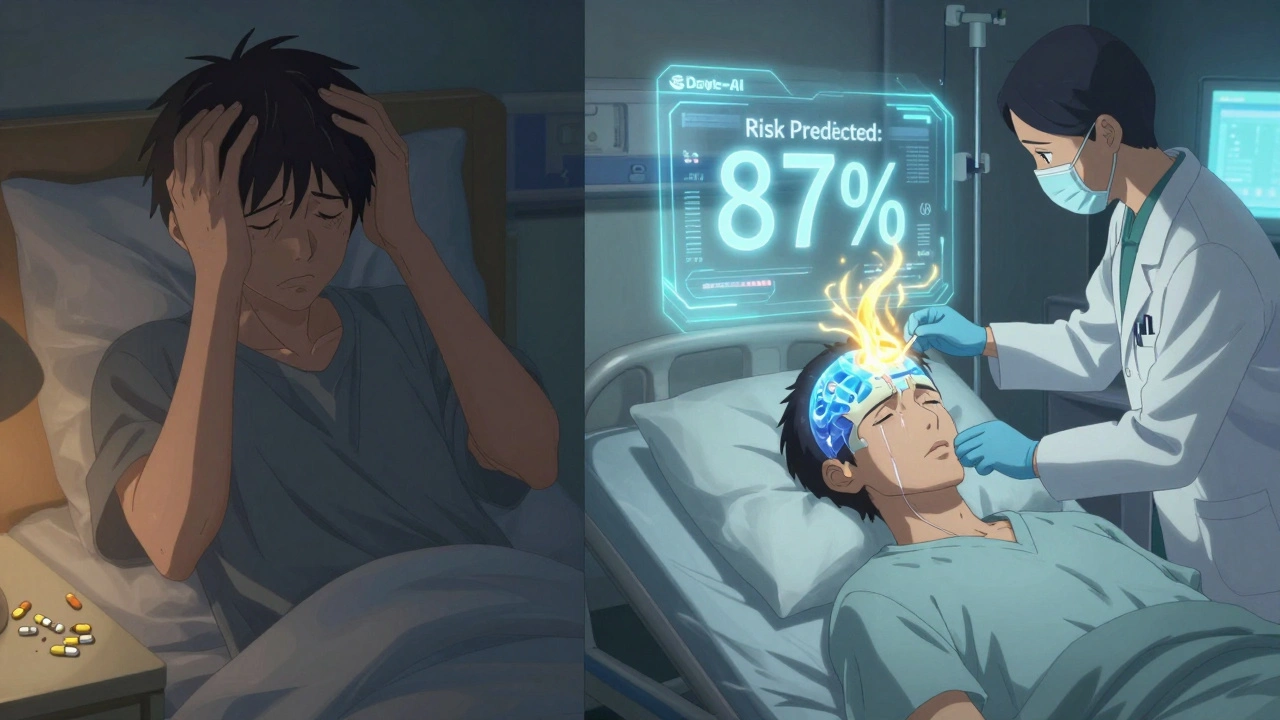
What’s Next? AI, Guidelines, and Hope
There’s progress. The European Medicines Agency now requires pharmacists to educate patients about sodium risks when dispensing high-risk drugs. Mayo Clinic is piloting an AI tool that scans electronic health records and predicts hyponatremia risk 72 hours before symptoms appear - with 87% accuracy. Imagine a system that flags a 70-year-old woman on sertraline and hydrochlorothiazide, then auto-schedules a blood test. No one has to remember. No one has to ask.
Models predict that with better screening, severe complications could drop by 38% by 2028. That’s tens of thousands of lives saved. But it won’t happen unless doctors, pharmacists, and patients all act.
The window between confusion and seizures can be as short as six to eight hours. That’s not a long time. But it’s enough - if you know what to look for.
Final Thought
You take a pill to feel better. You don’t expect it to make your brain swell. But it can. And it does - more often than you think. The good news? This condition is preventable. Detectable. Treatable. But only if you know the signs. Only if you ask. Only if someone in your care circle is paying attention.
Don’t wait for a seizure. Don’t wait for coma. Ask for a blood test. Before you start. After you start. If something feels off - get it checked. Your brain can’t wait.