More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the truth: penicillin allergy is often misdiagnosed. In fact, up to 95% of those who think they’re allergic can actually take penicillin safely - if they get tested. This isn’t just a minor mix-up. It affects your health, your treatment options, and even the spread of dangerous superbugs.
Why Most Penicillin Allergies Aren’t Real
If you were told as a kid you had a penicillin allergy because you got a rash after taking it, you’re not alone. That’s the most common reason people carry the label. But rashes from viruses, like the ones that come with colds or mononucleosis, often show up right after taking antibiotics. Doctors back then didn’t always know the difference. So the allergy label stuck. Fast forward to today, and research shows only about 1% of the population has a true penicillin allergy. That means 9 out of 10 people who say they’re allergic aren’t. The problem? Once you’re labeled, it’s hard to get it removed. Hospitals and clinics assume you’re allergic unless proven otherwise - even if it’s been 20 years since you took penicillin. The result? Doctors avoid penicillin and its close relatives (like amoxicillin and ampicillin), even though they’re the best, safest, and cheapest options for many infections. Instead, they reach for stronger, broader-spectrum antibiotics. These drugs don’t just cost more - they increase your risk of deadly infections like C. difficile and MRSA. One study found patients with a penicillin allergy label had a 50% higher chance of getting MRSA and a 35% higher chance of C. difficile.What a Real Penicillin Allergy Looks Like
Not all reactions are the same. There are two main types: immediate and delayed. Immediate reactions happen within an hour. These are the dangerous ones. They’re caused by IgE antibodies and can lead to anaphylaxis - a life-threatening response. Symptoms include swelling of the lips, tongue, or throat; trouble breathing; a sudden drop in blood pressure; dizziness; or passing out. If this has ever happened to you after taking penicillin, you need to see an allergist. Don’t take chances. Delayed reactions are more common - and usually less serious. They show up days after taking the drug. A flat, red rash that spreads over your body is the most typical sign. It might itch, but it’s not life-threatening. Other delayed reactions, like Stevens-Johnson Syndrome or DRESS, are rare but serious. These involve blistering skin, fever, and organ damage. If you’ve had one of these, you should avoid penicillin forever. The key? Know what happened to you. Was it a rash? A fever? Trouble breathing? Did it happen right after the pill, or three days later? Your history matters.How to Find Out If You’re Really Allergic
The only way to know for sure is through testing. And it’s simpler than you think. First, a skin test. A tiny amount of penicillin is placed under your skin. If you’re allergic, a red, itchy bump appears within 15-20 minutes. This test checks for IgE antibodies - the kind that cause anaphylaxis. If the skin test is negative, the next step is an oral challenge. You swallow a small dose of amoxicillin - the most common penicillin-type drug - and are watched for an hour. No reaction? You’re not allergic. That’s it. This whole process takes less than two hours. It’s done in a doctor’s office or clinic, not a hospital. No needles, no overnight stay. Just a safe, controlled way to remove a label that’s been holding you back. And here’s the best part: if you’ve avoided penicillin for more than 10 years, your body may have forgotten it ever reacted. About 80% of people lose their allergy over time. That’s why even if you had a reaction decades ago, testing is still worth it.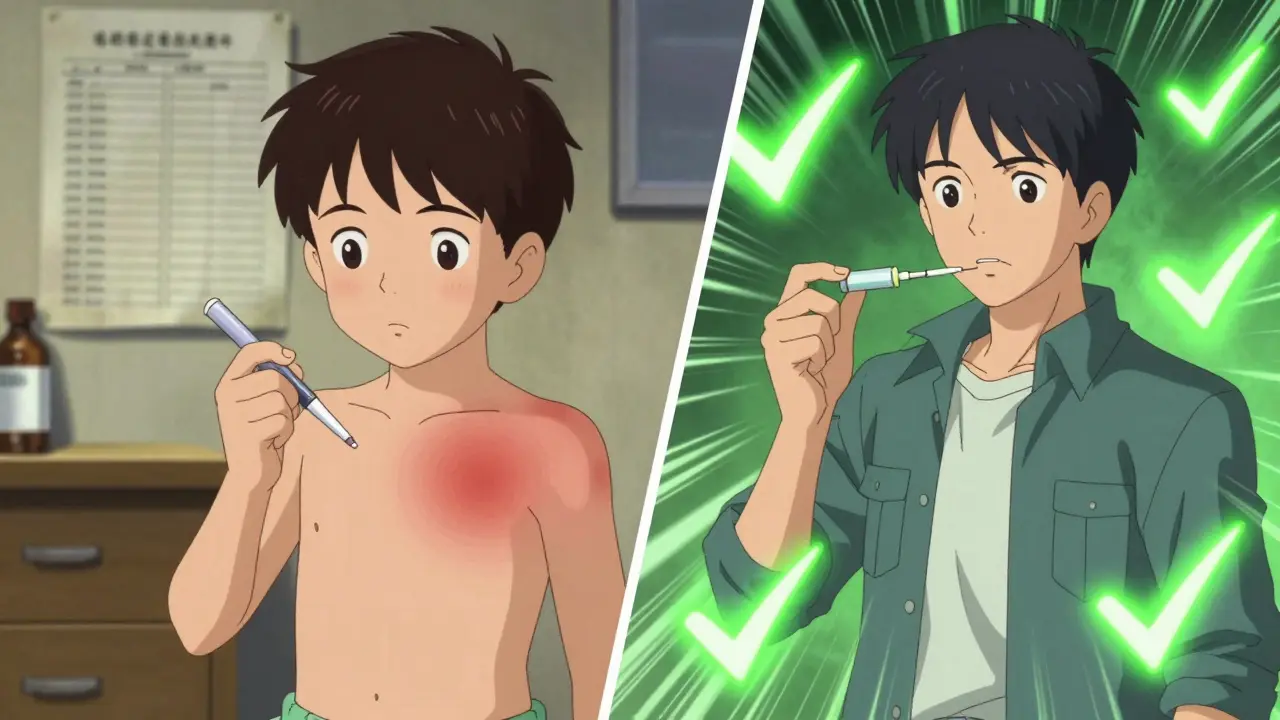
Who Can Skip Testing - and Who Can’t
Not everyone needs testing. Risk matters. Low-risk patients include people who had:- A rash that wasn’t itchy or spreading
- Stomach upset, headache, or dizziness - these are side effects, not allergies
- A reaction more than 5 years ago, especially if it was just a mild rash
- No clear history - like being told as a child, but never tested
- Hives or swelling within the last 5 years
- Any reaction that included trouble breathing or wheezing
- Swelling of the face or throat
What Happens After Testing?
If you test negative, you’re cleared. Not just for penicillin - for all beta-lactam antibiotics, including amoxicillin, ampicillin, and even some cephalosporins. Your doctor can now treat you with the best, most targeted drug. But here’s the catch: the label doesn’t disappear unless you make it happen. You need to ask your doctor to update your medical records. If you don’t, the next time you walk into a hospital or pharmacy, they’ll still see “penicillin allergy” - and treat you accordingly. Bring your test results. Ask them to remove the allergy from your chart. Tell your family. Update your phone’s medical ID. If you’re getting surgery, make sure your surgeon knows you’re cleared. One study found that for every 112 people tested, one surgical infection was prevented. That’s not just personal - it’s public health.
What to Do Right Now
If you’ve been told you’re allergic to penicillin:- Look back at your history. What exactly happened? When? How long ago?
- If it was a rash, stomach upset, or something more than 5 years ago - talk to your doctor about testing.
- If you had swelling, trouble breathing, or anaphylaxis - see an allergist. Don’t wait.
- If you’ve never been tested but carry the label - ask if you’re a candidate for a skin test and oral challenge.
- Once cleared, make sure your records are updated. Don’t assume someone else will do it.
Why This Matters Beyond You
Every time a doctor uses a broad-spectrum antibiotic because they think you’re allergic, they’re helping superbugs grow. Antibiotic resistance isn’t a distant threat. It’s here. It’s killing people. And it’s fueled by mislabeled allergies. The U.S. healthcare system loses $1.2 billion a year because of this. That’s money spent on longer hospital stays, stronger drugs, and preventable infections. It’s not just about you - it’s about everyone who might need antibiotics in the future. Getting tested isn’t just smart for your health. It’s a small act of responsibility for the whole system.What to Bring to Your Appointment
Before you go to your allergist or doctor:- Write down every antibiotic you’ve ever taken and what happened
- Bring old medical records if you have them
- Know the names of any drugs you took - don’t just say “that antibiotic from years ago”
- Ask if they offer penicillin skin testing and oral challenges
Can I outgrow a penicillin allergy?
Yes. About 80% of people who had an IgE-mediated penicillin allergy lose their sensitivity after 10 years without exposure. Even if you had a serious reaction as a child, you may be able to take penicillin safely now - if you get tested.
Is a rash always a sign of penicillin allergy?
No. Many rashes that appear after taking penicillin are caused by viruses, not the drug. A non-itchy, flat rash that shows up days later is often a viral reaction, not an allergy. True allergic rashes are raised, itchy, and appear quickly. Only testing can tell the difference.
Can I take other antibiotics if I’m allergic to penicillin?
It depends. If you’re truly allergic, you should avoid all penicillin-related drugs. But many people labeled allergic can safely take cephalosporins, carbapenems, or aztreonam - especially if they never had an IgE-mediated reaction. Testing opens up more options, not fewer.
How long does penicillin allergy testing take?
Usually less than two hours. Skin testing takes about 20 minutes, followed by an oral challenge with amoxicillin and one hour of observation. No hospital stay is needed. Most clinics offer this as a same-day appointment.
What if I’m allergic and need antibiotics now?
If you have a confirmed allergy and need treatment right away, doctors can use alternatives like clindamycin, vancomycin, or fluoroquinolones - depending on the infection. But these are often less effective, more expensive, and carry higher risks. Testing later can help you avoid them in the future.
Should I wear a medical alert bracelet?
Only if you’ve had a severe reaction - like anaphylaxis, Stevens-Johnson Syndrome, or DRESS. If you’ve never had a life-threatening reaction, a bracelet isn’t necessary. But if you’ve been told you’re allergic without testing, you don’t need one. Get tested first.
