Every winter, parents face the same exhausting cycle: a runny nose, a cough that won’t quit, sleepless nights - and the desperate urge to make it stop. So they reach for the bottle in the medicine cabinet. The label says Children’s Cold Medicine. It seems safe. It’s over-the-counter, after all. But here’s the truth most parents don’t know: giving those medicines to kids under 4 can land them in the hospital - and sometimes, it’s already too late.
Why OTC Cold Medicines Don’t Work for Young Kids
The idea that cough syrups and decongestants help little ones recover faster is a myth. Back in 2008, the U.S. Food and Drug Administration (FDA) reviewed every single study manufacturers had submitted. The result? No proof these medicines actually improved symptoms in children under 12. Not one. Not even a little. And yet, millions of doses were still being given each year. The active ingredients in these products - antihistamines like diphenhydramine, decongestants like pseudoephedrine, cough suppressants like dextromethorphan, and expectorants like guaifenesin - were never tested properly in young children. They were simply copied from adult formulas and scaled down by age, not weight. That’s a problem. A 2-year-old weighing 25 pounds and a 2-year-old weighing 35 pounds might look similar, but giving them the same dose based on age alone can lead to a 37% overdose risk, according to the American Academy of Pediatrics.The Real Danger: Overdose and Deadly Side Effects
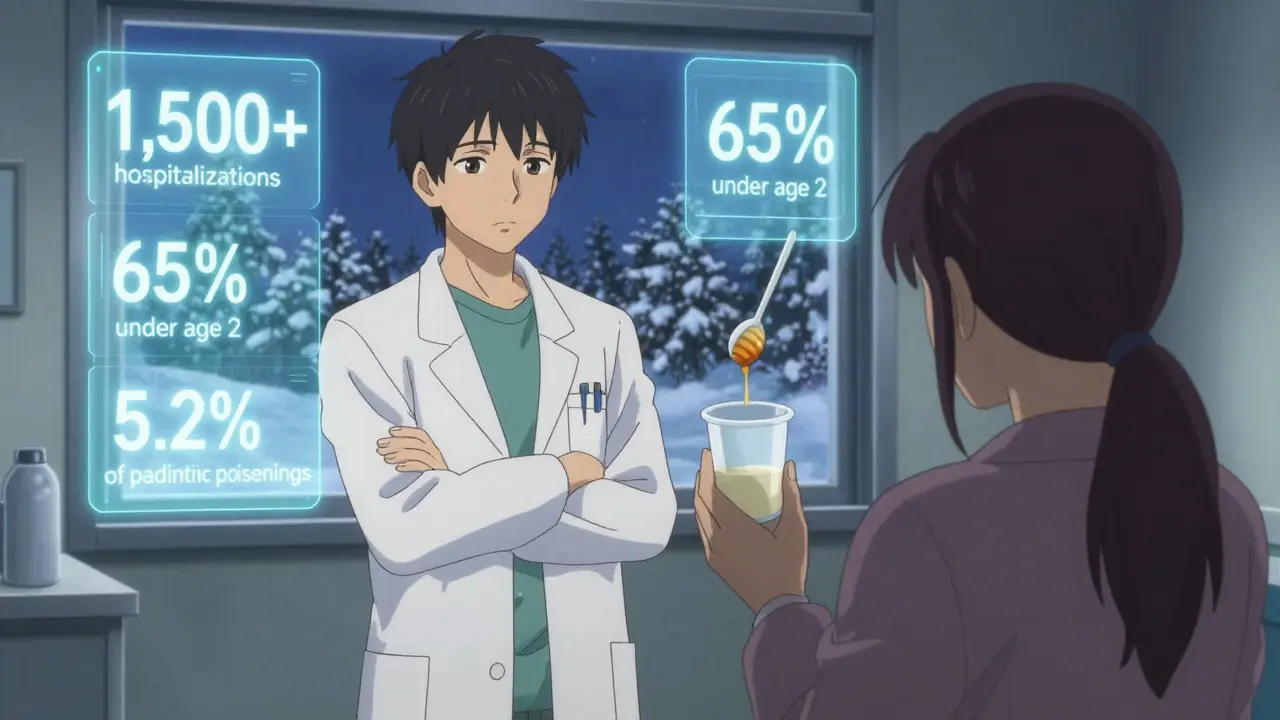
It’s not just that these medicines don’t work. They can kill. Between 2004 and 2015, more than 1,500 children were hospitalized because of reactions to OTC cold medicines. Over 65% of those cases involved kids under 2. Symptoms? Fast heartbeat, seizures, extreme drowsiness, trouble breathing. In some cases, children slipped into comas. A 2012 study found that 5.2% of all pediatric drug poisonings reported to the National Poison Data System came from these exact products. Most of these incidents weren’t from kids stealing pills. They were from well-meaning parents giving too much - because they didn’t know the right dose, or they gave another medicine with the same ingredient, or they used a kitchen spoon instead of the dosing cup. Multi-ingredient products are the worst offenders. One bottle might contain a cough suppressant, an antihistamine, and a decongestant - all in one. Give that to a toddler, and you’re stacking risks. Poison Control centers in the U.S. received over 12,000 calls between 2019 and 2022 about children exposed to these medicines. Nearly half involved kids aged 1 to 2. Over a third of those cases needed hospital treatment.The Official Age Limits - And Why They Exist
The FDA, along with the Consumer Healthcare Products Association (CHPA), says: Do not use OTC cough and cold medicines in children under 4 years old. That’s not a suggestion. That’s a safety rule backed by years of data. Manufacturers like Johnson & Johnson, GlaxoSmithKline, and Reckitt Benckiser have all updated their labels to say this clearly. But here’s the catch: some products now say “under 6” or even “under 12.” Why? Because some companies are going further - and some are just trying to cover themselves legally. The American Academy of Pediatrics (AAP) recommends avoiding these medicines entirely for kids under 6. The American Academy of Family Physicians gives them a “D” rating - meaning there’s high certainty the harm outweighs any benefit. Even the European Medicines Agency banned these products for kids under 6 in 2009. Switzerland went even further, banning dextromethorphan in all pediatric cough medicines as of January 2022. There’s one exception some experts point to: dextromethorphan in children aged 6 to 11. A few studies suggest it might help with coughing at night. But even that’s debated. Most doctors still say: skip it. The risk isn’t worth it.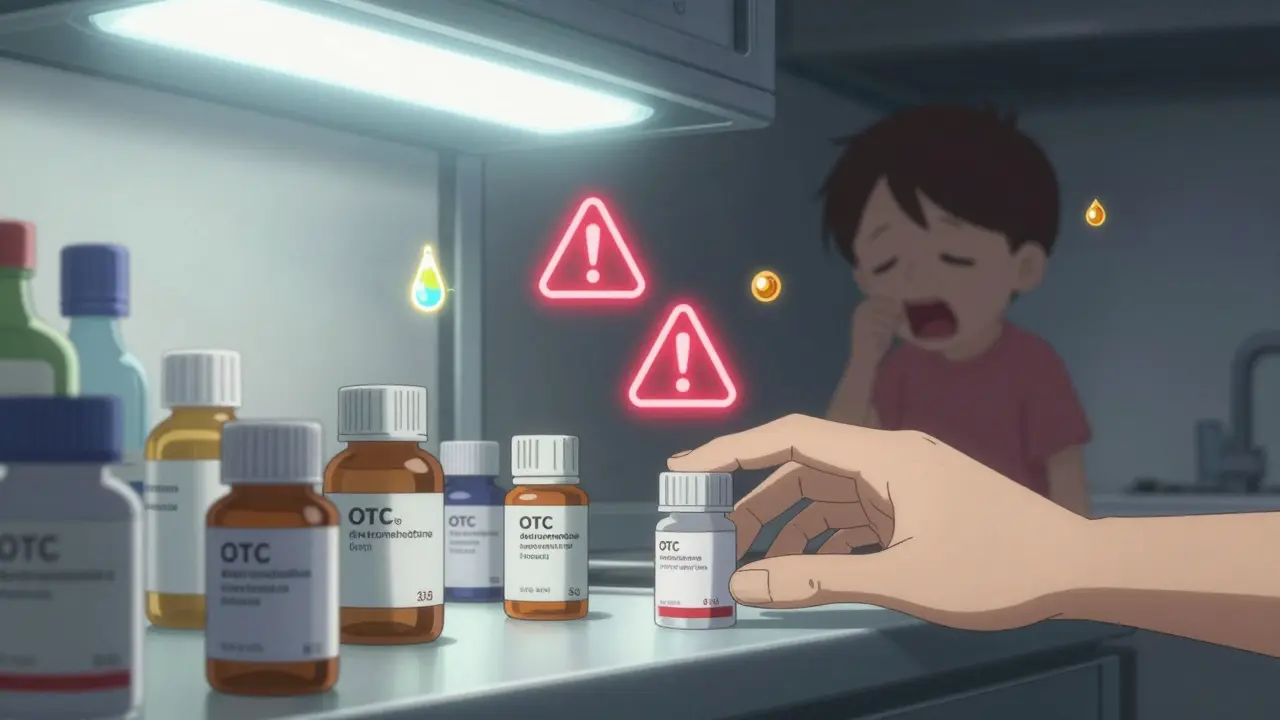
What Parents Are Really Doing (And Why)
Despite all the warnings, a 2021 AAP survey found that 38% of parents still give OTC cold medicine to kids under 4. Why? Because they’re desperate. One parent on Reddit wrote: “I gave my 2-year-old Robitussin DM against the label - he couldn’t sleep. I didn’t know what else to do.” And here’s the heartbreaking part: 62% of those parents said they did it because they thought their doctor recommended it. But when researchers checked medical records, only 17% had actually talked to a doctor. The truth? No pediatrician is prescribing these medicines to toddlers. They know the risks. But parents are left with no clear alternatives - and that’s where the confusion starts.What Actually Works: Safe, Proven Alternatives
You don’t need medicine to help a child feel better with a cold. Here’s what the AAP, CDC, and Cochrane reviews say actually helps:- Saline nasal drops - Use 2-3 drops in each nostril, then gently suction with a bulb syringe. Do this before meals and bedtime. It clears congestion without any drugs.
- Honey - For kids over 1 year old, give 2.5 mL (half a teaspoon) before bed. A 2018 Cochrane review found honey reduced cough frequency by 36% compared to placebo. It’s better than any syrup.
- Hydration - Offer water, breast milk, or formula more often. Kids need about 50 mL per kilogram of body weight extra each day when sick.
- Humid air - Run a cool-mist humidifier in the bedroom. Keep humidity between 40% and 60%. Moist air soothes irritated airways.
- Fever relief - If your child has a fever and is uncomfortable, use acetaminophen (10-15 mg/kg every 4-6 hours) or ibuprofen (5-10 mg/kg every 6-8 hours) - but only if they’re over 6 months old.
How to Avoid Mistakes - And Keep Your Child Safe
If you’re tempted to reach for that bottle, pause. Here’s how to stay safe:- Never mix medicines. Check every label. If two products have the same active ingredient, don’t use them together.
- Use only the dosing tool that comes with the bottle. A kitchen spoon holds way more than a teaspoon. Using the right tool cuts dosing errors by 47%.
- Store medicines out of reach. Most poisonings happen when kids find the bottle themselves. Lock it up.
- Don’t use adult medicine for kids. Even a small amount can be deadly.
- Call Poison Control immediately if you’re unsure. In the U.S., it’s 1-800-222-1222. They’re free, fast, and available 24/7.
What’s Changing - And What’s Coming
The market for pediatric OTC cold medicines has shrunk by nearly 30% since 2007. Over 37 brands were pulled from shelves after the FDA demanded proof they worked in kids. Today, only a few major brands remain - and they’ve all removed the lower age ranges. The FDA is now pushing for even stricter rules. Their 2023 draft guidance says all pediatric OTC drugs should go through clinical trials before being sold. Final rules are expected by mid-2025. Meanwhile, researchers at Nationwide Children’s Hospital are testing lower-dose versions for kids 2-4 years old. Early results show a 50% drop in adverse events with reduced doses. The future? More saline sprays, more humidifiers, more education - and fewer bottles of syrup in the cabinet.Bottom Line: Don’t Risk It
Colds are uncomfortable. They’re scary. But they’re not dangerous for most healthy kids. The real danger isn’t the virus - it’s the medicine you give to fight it. For kids under 4: Do not use OTC cold medicine. For kids 4-6: Avoid unless your pediatrician says otherwise. For older kids, stick to single-ingredient products and only if symptoms are severe. Your child doesn’t need a syrup to get better. They need rest, fluids, and a little patience. And you? You need to know that sometimes, the safest thing you can do is nothing at all.Can I give my 3-year-old Children’s Robitussin for a cough?
No. The FDA and manufacturers clearly state these products should not be used in children under 4 years old. Even if the bottle says "for ages 2+," that labeling is outdated or misleading. Giving Robitussin or similar products to a 3-year-old carries a risk of overdose, seizures, or respiratory depression. Use saline drops, honey (if over 1 year), and humidified air instead.
What if my child has a fever? Can I use fever medicine with cold medicine?
Don’t combine them. If your child has a fever, use acetaminophen or ibuprofen alone - and only if they’re over 6 months old. Many cold medicines already contain these pain relievers. Giving both can lead to accidental overdose. Always check the active ingredients on the label. If in doubt, skip the cold medicine entirely and treat only the fever.
Are natural or herbal cold remedies safe for kids?
Not necessarily. Many so-called "natural" products aren’t regulated like medicines. Some contain hidden ingredients like ephedrine or antihistamines. Others, like echinacea or elderberry, haven’t been proven safe or effective in children. Stick to what’s backed by science: saline, honey, hydration, and humidifiers. Avoid unregulated supplements.
Why do doctors still sell these medicines if they’re unsafe?
Most don’t. Pediatricians generally avoid recommending them. But some pharmacies still stock them, and some general practitioners may not be fully updated on the guidelines. The real issue is that parents are pressured by marketing, old habits, and desperation. The medicines are still on shelves - but that doesn’t mean they’re safe or recommended.
What should I do if my child accidentally takes too much?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Do not wait for symptoms to appear. Overdose can be silent at first. Have the medicine bottle ready when you call - the ingredients and amount taken matter. If your child is having trouble breathing, is unresponsive, or is having seizures, call 911 right away.
Is it okay to use OTC cold medicine for a 5-year-old?
The FDA recommends avoiding these medicines for children under 4. For 5-year-olds, the risk still outweighs the benefit. Some products say "for ages 4+," but even then, studies show little to no improvement in symptoms. If symptoms are mild, stick to saline, honey, and fluids. If your child has severe congestion or a persistent cough, talk to your pediatrician - don’t self-medicate.
What’s the difference between cough syrup and cold medicine?
Cough syrup usually targets just coughing (with dextromethorphan or honey). Cold medicine often combines multiple ingredients: cough suppressant, decongestant, antihistamine, and sometimes fever reducer. Multi-ingredient cold medicines are far more dangerous because they increase the chance of overdose. If your child only has a cough, avoid cold medicine entirely. Use honey (if over 1 year) or a humidifier instead.
Do pediatricians ever recommend OTC cold medicine?
Rarely - and only in very specific cases, like a child with chronic lung disease or severe nasal blockage that’s affecting feeding. Even then, they’ll usually recommend a single ingredient at the lowest possible dose. For healthy children with a common cold, pediatricians almost never recommend OTC cold medicine. If someone says their doctor said it’s okay, they may have misunderstood. Always double-check with your child’s doctor before giving any medicine.
