When you hear about mupirocin, you probably think of a simple skin ointment that clears up nasty infections. The truth is a bit more nuanced: even a topical drug can mingle with other medicines, and the right mix can mean the difference between a speedy heal and a stubborn rash.
Quick Takeaways
- mupirocin interactions are rare but matter when you combine it with other topical agents or systemic drugs that affect skin healing.
- Most concerns involve skin irritation, reduced antibacterial efficacy, or altered absorption.
- Always check for overlapping ingredients, especially other antibiotics, steroids, or immunosuppressants.
- Use the checklist below to verify safety before stacking treatments.
- If in doubt, consult a pharmacist or prescriber.
What Is Mupirocin?
mupirocin is a topical antibiotic derived from Pseudomonas fluorescens. It blocks bacterial protein synthesis by binding to isoleucyl‑tRNA synthetase, a mechanism that makes it especially potent against Staphylococcus aureus and its methicillin‑resistant strain (MRSA).
The drug comes in 2% ointment or 2% cream, intended for short‑term use on small skin lesions-think impetigo, minor cuts, or colonized wounds. Because it’s applied locally, systemic absorption is minimal, which is why most drug‑drug interaction warnings are light.
Why Interactions Still Matter
Even with low systemic exposure, two things can go wrong when you pair mupirocin with other products:
- Physical or chemical incompatibility: Mixing ointments can change the drug’s release rate or cause irritation.
- Pharmacodynamic overlap: Two agents fighting the same bacteria may be redundant, while adding a steroid could dampen the immune response needed for healing.
Understanding these pathways helps you avoid unnecessary side effects and keeps the infection under control.
Common Medications That May Interact
Below is a concise rundown of the most frequently co‑prescribed or over‑the‑counter (OTC) agents that clinicians should flag when they see a mupirocin prescription.
- Bacitracin - Another topical antibiotic. Using both can lead to increased local irritation without added benefit.
- Neomycin - Often found in triple‑antibiotic ointments. Overlap may heighten the risk of contact dermatitis.
- Hydrocortisone - A low‑potency corticosteroid. If applied together, the steroid may suppress the skin’s natural defense, potentially blunting mupirocin’s effect.
- Retapamulin - A newer topical antibiotic used for similar indications. Co‑administration is unnecessary and could cause skin dryness.
- Salicylic acid - Keratolytic agent used for wart removal. Acidic environments can degrade mupirocin’s active form.
- Cyclosporine - Systemic immunosuppressant (e.g., in transplant patients). While systemic interaction is minimal, the combined immunosuppression may impair wound healing.
- Warfarin - Oral anticoagulant. No direct interaction, but if skin integrity is compromised, bleeding risk rises, so monitor the wound closely.
Interaction Severity Table
| Co‑administered Agent | Interaction Type | Clinical Significance | Recommendation |
|---|---|---|---|
| Bacitracin | Physical | Mild irritation | Avoid simultaneous use; separate application times. |
| Hydrocortisone | Pharmacodynamic | Potential reduced efficacy | If needed, apply steroid after 30minutes of mupirocin absorption. |
| Salicylic acid | Chemical | Degradation of mupirocin | Do not layer; use separate treatment sites. |
| Cyclosporine | Pharmacodynamic (systemic) | Impaired wound healing | Monitor closely; consider alternate topical if healing stalls. |
| Warfarin | None (systemic only) | No direct effect | Standard wound care; watch for bleeding. |
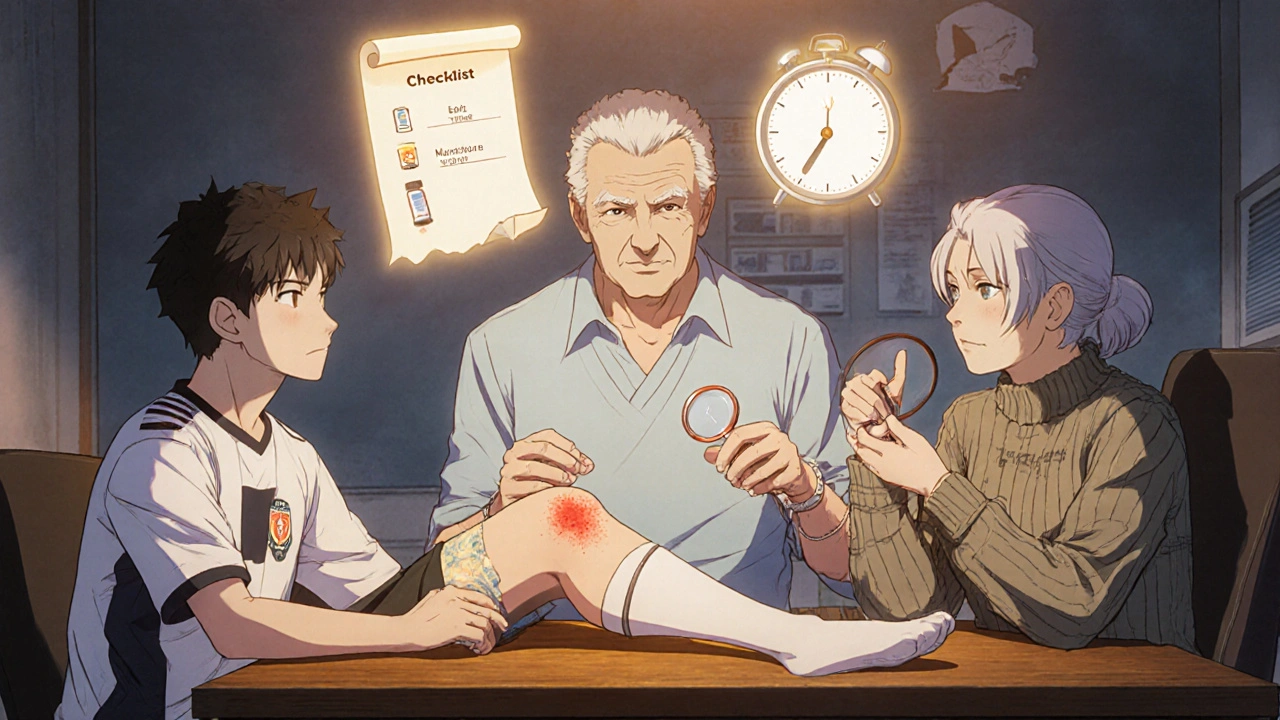
Practical Guidance for Clinicians
Here’s a step‑by‑step checklist you can keep on your desk before prescribing or dispensing mupirocin.
- Confirm the indication - impetigo, minor abscess, or MRSA colonization.
- Review the patient’s medication list for any of the agents in the table above.
- If a topical antibiotic (bacitracin, neomycin) is already in use, advise a wash‑out period of at least 12hours before applying mupirocin.
- When a steroid is required, instruct the patient to apply mupirocin first, let it absorb (≈30min), then apply the steroid.
- For patients on systemic immunosuppressants (cyclosporine, tacrolimus), schedule a follow‑up at day5 to assess healing.
- Document any concurrent OTC products (e.g., acne creams) that contain salicylic acid or benzoyl peroxide.
- Educate the patient to report severe redness, swelling, or new pain, which could signal a reaction.
Real‑World Scenarios
Case 1 - The Athlete: A 22‑year‑old soccer player with a small impetigo lesion also uses a topical antifungal cream for athlete’s foot. The antifungal contains miconazole, which does not chemically interfere with mupirocin. The clinician recommends applying mupirocin in the morning and the antifungal at night, avoiding direct overlap on the same skin patch.
Case 2 - The Transplant Recipient: A 55‑year‑old liver transplant patient on cyclosporine develops a superficial MRSA wound. Because systemic immunosuppression slows healing, the physician adds mupirocin but schedules weekly wound assessments. No additional topical steroids are used, preserving the drug’s antibacterial action.
Case 3 - The Elderly Diabetic: An 78‑year‑old with type‑2 diabetes uses over‑the‑counter hydrocortisone 1% for eczema flare‑ups near a minor laceration. The pharmacist advises applying mupirocin first, waiting 30minutes, then applying hydrocortisone, ensuring the antibiotic can act unhindered.
Checklist for Patients
- Read the label - confirm it says 2% mupirocin ointment or cream.
- Wash the affected area gently before each application.
- Apply a thin layer; more does not mean faster healing.
- Wait at least half an hour before using another cream or ointment on the same spot.
- Do not cover the area with tight dressings unless instructed.
- Complete the full course (usually 5‑10 days) even if the skin looks better.
- Report any rash, itching, or worsening redness immediately.
Key Takeaway for Pharmacists
Because mupirocin is topical, the biggest interaction red flags are other skin products, not systemic drugs. Keep an eye on overlapping topical antibiotics, steroids, and acidic agents. A quick medication review and clear counseling can prevent most problems.
Frequently Asked Questions
Can I use mupirocin and a steroid cream at the same time?
Yes, but apply the mupirocin first and let it absorb for about 30 minutes before putting on the steroid. This order prevents the steroid from blocking the antibiotic’s action.
Do oral antibiotics affect how mupirocin works?
Generally no. Because mupirocin stays on the skin, oral meds rarely change its potency. However, if you’re on a strong systemic antibiotic that also targets the same bacteria, you might be duplicating therapy without added benefit.
Is it safe to use mupirocin while taking warfarin?
There’s no direct drug‑drug interaction. The caution is to monitor the wound for bleeding, especially if the skin is broken and the patient is on warfarin.
What should I do if my skin becomes more red after applying mupirocin?
A mild increase in redness can be normal as the infection clears. If you experience intense burning, swelling, or spreading rash, stop the ointment and seek medical advice right away.
Can I apply mupirocin on an open surgical wound?
Mupirocin is approved for superficial skin infections. For deeper surgical wounds, follow the surgeon’s specific antibiotic protocol - usually a systemic agent rather than a topical ointment.
