Levothyroxine Dose Adjustment Calculator
This tool estimates the potential increase in levothyroxine dose required when taking proton pump inhibitors (PPIs). Based on clinical evidence, 15-20% of patients need dose adjustments due to reduced absorption.
Estimated Adjustment
Required dose increase: mcg
New target dose: mcg
Based on clinical studies showing 12.5-25 mcg average increase (15-20% of current dose)
Next step: Get TSH testing after 6-8 weeks. Consult your doctor before changing doses.
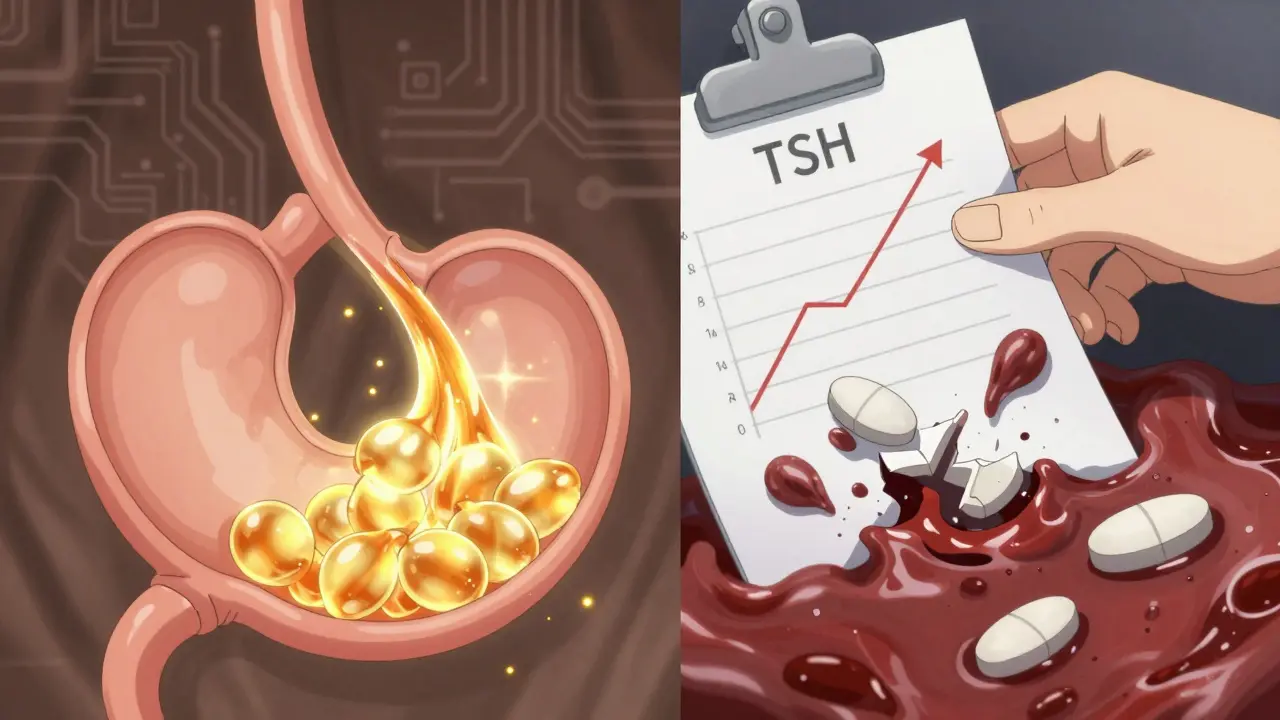
If you're taking levothyroxine for hypothyroidism and also use a proton pump inhibitor (PPI) for heartburn or acid reflux, you might be unaware that these two medications are working against each other. It’s not a matter of one causing side effects - it’s about your body not absorbing the thyroid hormone properly. And that can mean your TSH levels creep up, your fatigue gets worse, and your weight won’t budge - even if you’re taking your pills exactly as prescribed.
Why Levothyroxine Needs Acid
Levothyroxine isn’t like most pills that just dissolve and get absorbed. It needs an acidic environment in your stomach to break down and enter your bloodstream. The ideal pH for absorption is between 1 and 2 - that’s as acidic as vinegar. This is why doctors tell you to take it on an empty stomach, first thing in the morning, with a full glass of water. No coffee, no food, no supplements for at least 30 to 60 minutes. But if you’re also taking a PPI like omeprazole (Prilosec), esomeprazole (Nexium), or pantoprazole (Protonix), you’re essentially turning your stomach into a neutral pond.
PPIs shut down the acid pumps in your stomach lining. They’re powerful. One dose can keep your stomach pH above 4 for up to 24 hours. And for some, the effect lasts even longer. When your stomach pH rises to 4 or higher, levothyroxine doesn’t dissolve properly. It passes through your gut mostly unchanged. Your body doesn’t get the hormone it needs. So your thyroid-stimulating hormone (TSH) rises - your body’s signal that it’s still starving for thyroid hormone.
The Evidence Isn’t Theoretical - It’s Measurable
A 2021 systematic review in the Journal of General Internal Medicine looked at seven studies involving over 1,200 patients on both levothyroxine and PPIs. Every single one showed higher TSH levels when the drugs were taken together. In most cases, the increase was statistically significant. That means it wasn’t random. It was real.
One 2023 study followed patients taking 40 mg of pantoprazole daily for six weeks. These were people whose thyroid levels were perfectly stable on levothyroxine. After just six weeks on the PPI, their TSH jumped - even when they took the PPI at night and levothyroxine in the morning. Timing didn’t help. Because PPIs don’t just reduce acid for a few hours - they suppress it for days. Your stomach doesn’t bounce back quickly.
According to the Mayo Clinic, about 15% to 20% of people on both medications need their levothyroxine dose increased. On average, that’s an extra 12.5 to 25 micrograms per day. That’s not a small change. For someone on 75 mcg, that’s a 33% increase. And it’s not always obvious. You might feel fine - until you don’t.

What Symptoms Show Up When Absorption Fails
When levothyroxine isn’t absorbed, your body acts like it’s hypothyroid again. The symptoms are the same as when you were first diagnosed:
- Constant fatigue, even after sleeping
- Unexplained weight gain, despite eating the same
- Brain fog - trouble focusing, memory lapses
- Feeling colder than usual
- Dry skin, hair thinning
- Depressed mood or irritability
On Reddit’s r/Hashimotos community, over 140 patients shared their experiences in late 2023. Nearly 70% said their levothyroxine dose had to be increased after starting a PPI. Over 70% reported worsening fatigue. More than half said they gained weight they couldn’t lose. These aren’t anecdotes. They’re patterns backed by lab results.
What You Can Do - Practical Solutions
There are four real-world ways to fix this - and not all of them involve higher doses.
1. Switch to Liquid Levothyroxine
There’s a formulation called Tirosint-SOL. It’s not a tablet. It’s a liquid in a softgel capsule. It contains glycerin, not fillers like lactose or cornstarch. And critically, it doesn’t need stomach acid to be absorbed. A 2019 study in the Journal of Clinical Endocrinology & Metabolism showed that patients on Tirosint-SOL had stable TSH levels even while taking PPIs.
The catch? It costs about $350 a month. Generic levothyroxine is $15 to $25. Insurance doesn’t always cover the liquid version unless you’ve tried and failed with tablets. But for people who’ve struggled with absorption for years, it’s life-changing.
2. Try an H2 Blocker Instead
PPIs aren’t the only acid reducers. Famotidine (Pepcid) and ranitidine (though mostly off the market now) are H2 receptor antagonists. They work differently - they block histamine receptors, not acid pumps. They’re less potent, but they don’t suppress acid for days. A 2018 study in Pharmacotherapy found no significant change in TSH when patients took famotidine with levothyroxine.
If you only need acid control for occasional heartburn, H2 blockers are a better fit. They’re cheaper, available over the counter, and don’t wreck your thyroid absorption. But if you have severe GERD or Barrett’s esophagus, they might not be strong enough.
3. Don’t Rely on Timing Alone
You’ve probably heard: “Take your PPI at night, levothyroxine in the morning.” That sounds logical. But here’s the problem: PPIs don’t just work for a few hours. Their effect lasts 24 to 72 hours, depending on the drug and your metabolism. A 2023 study specifically tested this - giving pantoprazole in the evening and levothyroxine at 6 a.m. - and still found TSH rose. The suppression is too long-lasting. Separating them by 4 hours, 8 hours, or even overnight doesn’t fix it.
4. Monitor TSH - and Adjust
If you’re stuck with a PPI - maybe you have ulcers or chronic GERD - then you need to test your TSH. The American Association of Clinical Endocrinologists recommends checking your TSH before starting the PPI, then again at 6 to 8 weeks. If it’s up, increase your levothyroxine by 12.5 to 25 mcg. Repeat every 6 weeks until levels stabilize. About 43% of patients reach stable TSH within 12 weeks, according to Cleveland Clinic data.
Don’t wait for symptoms to get bad. Get tested. Your doctor might not bring it up - but you should.
What’s Changing - and What’s Coming
This interaction isn’t new, but it’s finally getting attention. The FDA issued draft guidance in 2023 asking drugmakers to add clear warnings about PPI interactions on levothyroxine labels. That’s a big deal. It means regulators now recognize this as a widespread, clinically important issue.
Researchers are also testing new formulations - enteric-coated tablets designed to dissolve in the small intestine, not the stomach. If they work, they could be a game-changer. But they’re still in phase 3 trials.
Meanwhile, Tirosint-SOL’s patent expires in 2025. That could bring down the price dramatically. Generic manufacturers are already working on it, but reformulating levothyroxine without acidic absorption requirements is technically hard. It’s not just copying a tablet - it’s redesigning how the drug behaves in your body.
Bottom Line: This Is Manageable
You don’t have to choose between managing your thyroid and managing your stomach. But you do need to be proactive. If you’re on both medications:
- Ask your doctor to check your TSH within 8 weeks of starting the PPI
- Ask if switching to famotidine is an option
- Ask about Tirosint-SOL - especially if your dose keeps needing to go up
- Don’t assume your symptoms are just aging or stress
Levothyroxine works - if your body can absorb it. PPIs make that harder. But with the right steps, you can fix it. You don’t have to live with fatigue and weight gain because your meds are fighting each other.
