When you have inflammatory bowel disease (IBD) and are planning a pregnancy, the biggest question isn’t just IBD pregnancy - it’s whether your meds will keep you safe, and if they might hurt your baby. The truth? The biggest danger isn’t your medication. It’s uncontrolled disease.
Why staying in remission matters more than stopping meds
If your Crohn’s or ulcerative colitis is active when you get pregnant, your risk of complications jumps significantly. Studies show women with active IBD at conception are 2.3 times more likely to have a preterm baby, 1.8 times more likely to have a low-birth-weight infant, and 1.6 times more likely to experience stillbirth than those in remission. That’s not a small risk. It’s the kind of risk that changes how you plan your pregnancy. Many women panic at the thought of taking biologics or immunosuppressants while pregnant. But here’s the thing: stopping your meds to be "safe" often backfires. Stopping anti-TNF drugs like adalimumab or infliximab leads to flare-ups in over 60% of cases within six months. And when you flare, your body is under stress - inflammation affects blood flow to the placenta, hormone balance, and nutrient delivery to the fetus. That’s worse than any medication. The global Helmsley PIANO consensus, published in August 2023 after reviewing over 1,500 pregnancies, says it plainly: Women should aim for clinical and endoscopic remission on a steroid-free regimen for at least three months before conceiving. That’s not a suggestion. It’s the standard of care.Medications that are safe to keep taking
Not all IBD drugs are created equal when it comes to pregnancy. Some are proven safe. Others aren’t. Here’s what the latest data says.Aminosalicylates (5-ASAs): Mesalamine and Sulfasalazine
These are the oldest, most studied drugs for IBD. Both mesalamine and sulfasalazine are considered safe throughout pregnancy by the Crohn’s & Colitis Foundation and the European Crohn’s and Colitis Organisation (ECCO). But there’s a catch with mesalamine. Some formulations - like Asacol® - use a coating called dibutyl phthalate (DBP). Animal studies and human case reports link DBP to genital malformations in male babies. So if you’re on mesalamine, check the brand. Lialda, Delzicol, Apriso, and Mesalamine ER don’t contain DBP. Switch if needed. Sulfasalazine is also safe, but it blocks folate absorption. That’s why your doctor will likely prescribe a higher dose of folic acid - at least 1 mg daily, sometimes up to 5 mg - starting before conception. Folate deficiency increases the risk of neural tube defects. Don’t skip this step.Anti-TNF agents: Infliximab, Adalimumab, Certolizumab
These are the most trusted biologics in pregnancy. The PIANO registry tracked over 2,000 pregnancies exposed to anti-TNF drugs. Results? No increase in birth defects, preterm birth, or low birth weight compared to the general population. The rate of major congenital anomalies was 2.6%, nearly identical to the 2.8% baseline. Certolizumab (Cimzia) is unique. It doesn’t cross the placenta well because it lacks an Fc portion. That means less drug reaches the baby. Some doctors prefer it in the third trimester to reduce infant exposure. But infliximab and adalimumab are still considered safe. In fact, continuing them through delivery is recommended - especially if you’re at risk of a flare.Vedolizumab and Ustekinumab
Vedolizumab (Entyvio) is a gut-selective biologic. Early data from the CONCEIVE study raised a red flag: lower live birth rates. But when researchers removed women who had active disease during pregnancy, the numbers normalized. That tells you the real problem wasn’t the drug - it was inflammation. Ustekinumab (Stelara) has now been studied in over 680 pregnancies. No increase in birth defects, preterm birth, or low birth weight. A 2024 European study of 78 infants found no difference in outcomes whether the mom was on induction or maintenance therapy. Both drugs are now classified as Category B - limited but reassuring data.Medications to stop before pregnancy
Some drugs are outright dangerous. No exceptions.Methotrexate and Thalidomide
These are Category X - absolute contraindications. Methotrexate causes severe birth defects in 17-27% of exposed pregnancies. Thalidomide is infamous for limb deformities. If you’re on either, you must stop at least three months before trying to conceive. Your gastroenterologist should help you switch to a safer option.JAK inhibitors: Tofacitinib and Upadacitinib
These newer oral drugs work differently. Tofacitinib (Xeljanz) has data from just 11 pregnancies - too few to say it’s safe. The 2023 Crohn’s & Colitis Foundation guidelines recommend stopping it at least one week before conception. But most experts advise stopping it three months out, just to be safe. Upadacitinib (Rinvoq) has 98 prospectively followed pregnancies with no red flags - but the ECCO 2024 guidelines still recommend stopping it 4-6 weeks before conception. Why? Because JAK inhibitors interfere with the JAK-STAT pathway, which is critical in early embryonic development. The risk might be low, but the data isn’t enough to say it’s safe. Play it cautious.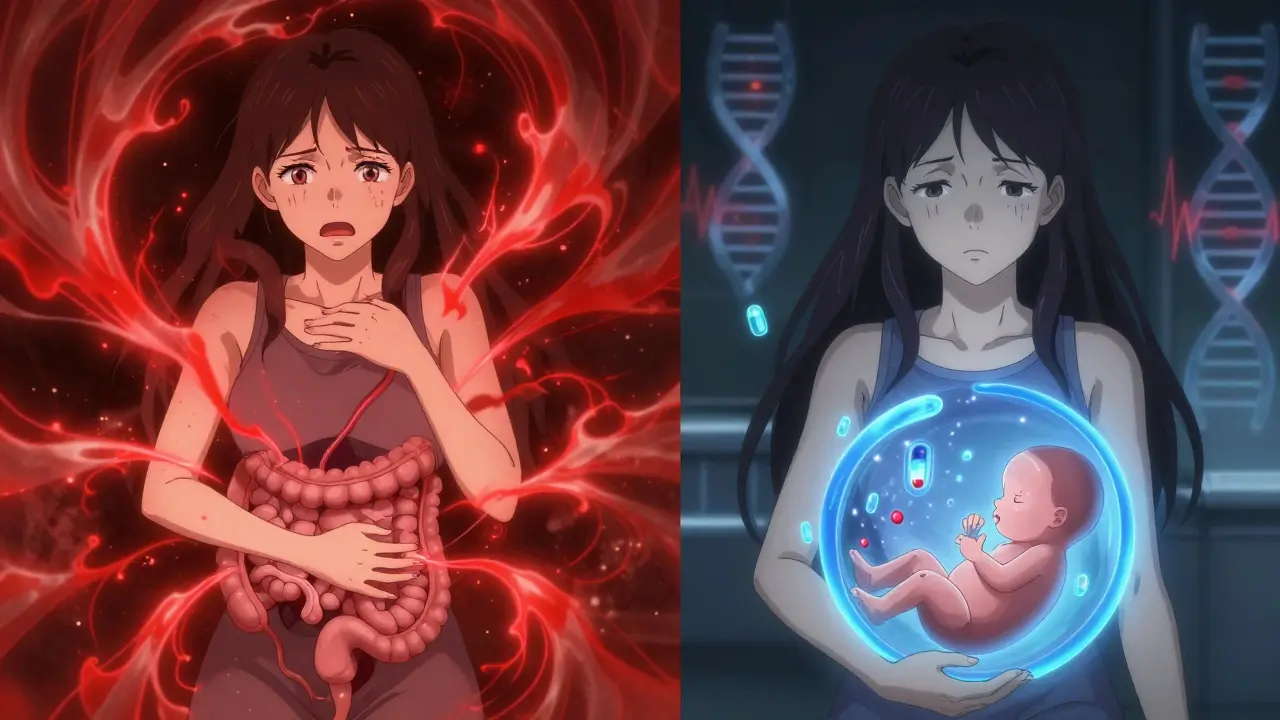
What about steroids and immunomodulators?
Corticosteroids: Prednisone, Budesonide
Steroids are a last resort. They work fast, but they’re not ideal in pregnancy. Taking oral steroids during the first trimester increases the risk of oral clefts by 1.4 to 2.3 times. Budesonide (Entocort) is safer - it’s broken down quickly in the liver, so less reaches the baby. Still, the goal is to avoid steroids entirely. Use them only for flares, and switch back to your maintenance meds as soon as possible.Azathioprine and 6-MP
These immunomodulators are safe to continue. Studies of over 1,000 pregnancies show no increased risk of birth defects. The key is monitoring your blood counts. These drugs can lower white blood cells. Your doctor should check your CBC every 2-4 weeks during pregnancy. Don’t stop them unless your counts crash - and even then, they’re often restarted at a lower dose.What happens after birth?
You’re not done after delivery. Breastfeeding is safe with almost all IBD meds. Anti-TNFs, vedolizumab, ustekinumab, azathioprine, and mesalamine all pass into breast milk in tiny amounts - far below therapeutic levels. The American Academy of Pediatrics considers them compatible with breastfeeding. Sulfasalazine? It can turn breast milk orange and might affect a baby’s gut flora. Some guidelines say monitor the baby for diarrhea or rash. Others say it’s fine. Most moms continue without issue. Vaccines? Yes, your baby can get all routine shots - even live ones like MMR and varicella. Exposure to biologics in utero doesn’t make your baby immunocompromised. The ECCO 2024 guidelines confirm this.
How to plan ahead
This isn’t something you figure out after a positive pregnancy test. You need a plan months in advance.- See your gastroenterologist at least 3-6 months before trying to conceive.
- Get a colonoscopy if you’re not in remission. Endoscopic healing matters as much as symptom relief.
- Switch to DBP-free mesalamine if needed.
- Start high-dose folic acid (1-5 mg/day).
- Stop methotrexate, thalidomide, or JAK inhibitors early.
- Coordinate care between your GI and OB-GYN. Shared care improves outcomes.