Every year, over 1.3 million people in the U.S. end up in the emergency room because of bad reactions to their medications. Many of these cases aren’t caused by faulty prescriptions or pharmacy errors-they happen because people are taking too many pills, not eating right, sleeping poorly, or skipping movement. The truth is, medication risks don’t have to be inevitable. You don’t need to stop your meds. You just need to change how you live.
Why Lifestyle Changes Work Better Than You Think
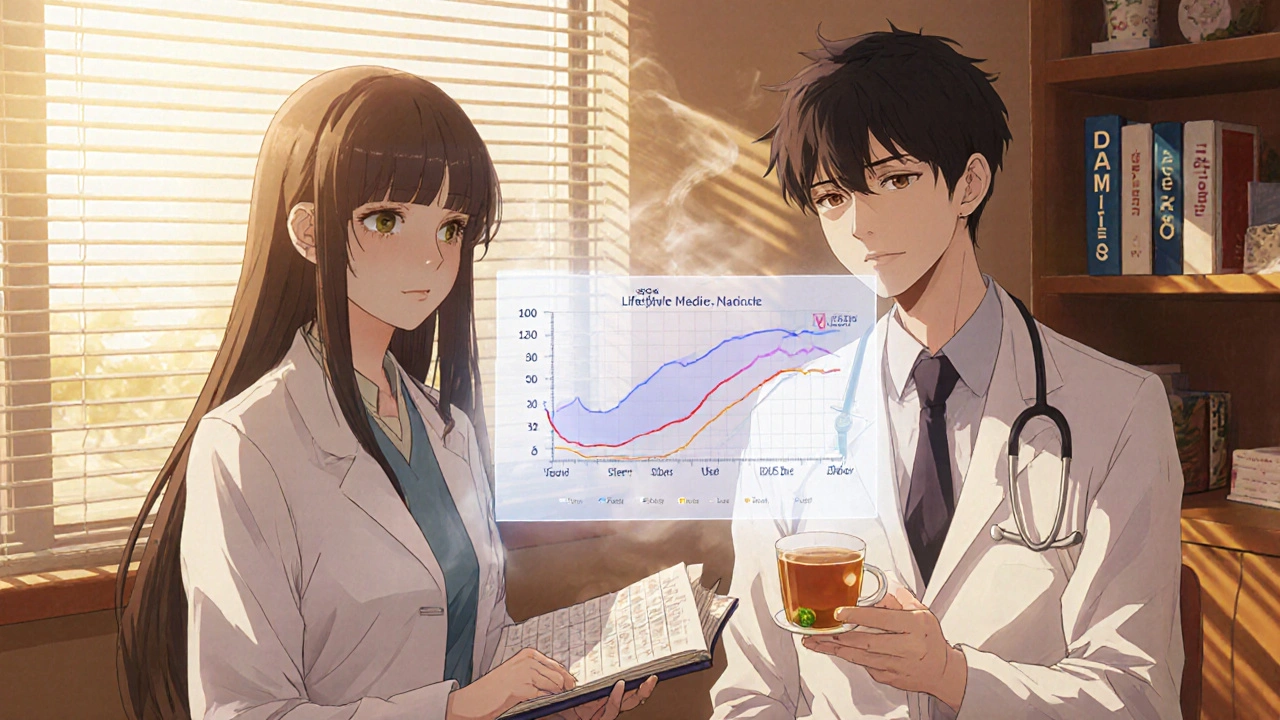
Medications treat symptoms. Lifestyle changes fix the root causes. If you have high blood pressure, a pill lowers it. But if you walk 30 minutes three times a week, reduce salt, and sleep seven hours a night, your heart gets stronger. That means your body might need less of the pill-or none at all. A 2023 study of 3.4 million people showed that people who made these changes cut their need for medication by 25% to 50% for conditions like diabetes, high cholesterol, and hypertension. This isn’t theory. It’s clinical fact. The American College of Lifestyle Medicine, founded in 2004, has spent two decades proving that diet, movement, sleep, and stress management aren’t just "nice to have"-they’re essential parts of treatment. And doctors are starting to listen. Medicare Advantage plans now cover some lifestyle programs. The FDA is asking drug companies to prove their pills work better when paired with lifestyle changes.The Big Four: Sleep, Movement, Food, and Stress
There are four pillars that make the biggest difference in reducing medication risks. Get these right, and you’re not just avoiding side effects-you’re reversing damage.- Sleep: Adults need 7 to 9 hours every night. Skimping on sleep raises your blood pressure, spikes blood sugar, and makes you hungrier for junk food. One study found that people who slept less than six hours were 20% more likely to need insulin for diabetes. Fix your sleep, and you might lower your dose-or even stop it.
- Movement: You don’t need to run marathons. Brisk walking for 30 minutes, three days a week, improves heart function enough to lower blood pressure like a pill. The American Heart Association recommends 150 minutes of moderate activity weekly, plus two days of strength training. That’s just 25 minutes a day. Do it consistently, and your body starts needing less medication to do the same job.
- Food: What you eat directly affects how your meds work. For high blood pressure, cutting sodium to under 1,500 mg a day lowers pressure as much as a single pill. For diabetes, eating more fiber, less sugar, and fewer processed carbs can improve blood sugar control better than some medications. The DASH diet (Dietary Approaches to Stop Hypertension) has been proven to lower systolic blood pressure by 11 points. That’s the same effect as lisinopril or hydrochlorothiazide.
- Stress: Chronic stress raises cortisol, which spikes blood sugar and blood pressure. Yoga, meditation, or even 10 minutes of deep breathing daily can lower stress hormones enough to reduce the need for beta-blockers or antidepressants. A 2023 VA study found that people with diabetes who practiced stress management along with their GLP-1 medication cut their heart attack risk by nearly half.
Real People, Real Results
One Reddit user, "HypertensionWarrior," had blood pressure of 150/95. After six months of daily walks and cutting salt from 3,500 mg to 1,500 mg, it dropped to 125/80. Their doctor took them off one pill. Another person, "DiabetesJourney," struggled with the social isolation of eating differently-but still lost 8% of their body weight and cut their metformin dose in half. These aren’t outliers. A 2024 survey of 2,400 people with chronic conditions found that 68% felt better, had fewer side effects, and needed fewer pills after making lifestyle changes. The catch? It takes time. You won’t see results in a week. Most people need 8 to 12 weeks of consistent effort before their body responds.
What Foods Can Interfere With Your Meds?
Lifestyle changes aren’t just about eating more veggies. Some healthy foods can clash with your pills.- Grapefruit: It interferes with 85% of statins (cholesterol drugs). Even one glass can make your body absorb too much of the drug, raising your risk of muscle damage.
- Leafy greens: Spinach, kale, and broccoli are full of vitamin K, which can make blood thinners like warfarin less effective. You don’t need to avoid them-just eat the same amount every day so your doctor can adjust your dose.
- Dairy: Milk and yogurt can block absorption of antibiotics like tetracycline and ciprofloxacin. Take these meds two hours before or after eating dairy.
- Alcohol: Mixing alcohol with painkillers, sedatives, or antidepressants can cause dizziness, liver damage, or breathing problems. Stick to one drink a day for women, two for men-if you drink at all.
Don’t Stop Your Meds-Talk to Your Doctor
Never quit or reduce your medication just because you feel better. Abruptly stopping blood pressure pills can cause a dangerous spike. Stopping insulin without a plan can lead to diabetic ketoacidosis. Lifestyle changes work best when they’re paired with your current treatment-not replacing it. Your doctor and pharmacist are your partners. Ask them:- "Can my diet or supplements affect how my meds work?"
- "Are there any medications I might be able to reduce if I stick with these changes?"
- "What’s the safest way to track progress?"
How Long Until You See Results?
Here’s what to expect:- Weeks 1-4: You’ll notice better energy, less brain fog, and improved sleep. Blood pressure and blood sugar may not change yet.
- Weeks 5-8: Your body starts adapting. You might feel less hungry, more motivated. Some people see small drops in blood pressure or glucose.
- Weeks 9-12: Measurable changes kick in. Studies show most people start seeing 10-20% improvement in lab values by this point.
- Months 4-6: This is when medication reductions often happen. If you’ve been consistent, your doctor might suggest lowering a dose.
What If You Can’t Stick With It?
Change is hard. You’re not failing-you’re human. Start small. Pick one thing. Maybe it’s walking after dinner three times a week. Or swapping soda for sparkling water. Or setting a phone alarm to turn off screens an hour before bed. One change leads to another. A 2024 UC Davis study found that people who used a simple app to track sleep and movement were 47% more likely to stick with their plan than those who just tried to remember. You don’t need to be perfect. You just need to be consistent. Miss a day? Get back on track the next. The goal isn’t to be flawless-it’s to be better than you were last month.The Bigger Picture: Why This Matters
Taking five or more medications-called polypharmacy-tripling your risk of dangerous side effects. That’s not just scary-it’s common. One in three older adults takes five or more pills daily. Many of those meds are for conditions that could’ve been prevented or reversed with lifestyle changes. The economic impact is huge. Medications make up nearly 18% of U.S. healthcare spending. Lifestyle programs cost a fraction of that-and they work. Employers who offer wellness programs see an 18.7% drop in chronic disease costs. Hospitals are starting to pay for nutritionists and fitness coaches because they save money in the long run. This isn’t about willpower. It’s about science. Your body was built to move, eat real food, rest deeply, and live without constant stress. Modern medicine treats symptoms. Lifestyle medicine treats the cause. Together, they’re the most powerful combo you’ve got.Can lifestyle changes replace my medication?
No-not without your doctor’s approval. Lifestyle changes should be added to your treatment plan, not used as a replacement. Stopping medication suddenly can be dangerous. But with consistent effort, your doctor may be able to lower your dose over time.
How long does it take for lifestyle changes to lower blood pressure or blood sugar?
You might notice small improvements in energy and sleep within a few weeks. Measurable changes in blood pressure or glucose levels usually appear after 8 to 12 weeks of consistent effort. Most people see the strongest results after 4 to 6 months.
Do I need to follow a special diet like keto or vegan to reduce medication risks?
No. You don’t need extreme diets. The DASH diet and Mediterranean-style eating-rich in vegetables, whole grains, lean protein, and healthy fats-are proven to help. Focus on reducing sugar, salt, and processed foods. Consistency matters more than perfection.
Can grapefruit really mess up my cholesterol pill?
Yes. Grapefruit interferes with how your body breaks down 85% of statins, causing too much of the drug to build up in your system. This raises your risk of muscle damage. Avoid grapefruit and grapefruit juice entirely if you’re on a statin. Talk to your pharmacist about alternatives.
What if I can’t afford healthy food or gym membership?
You don’t need expensive options. Frozen vegetables are just as nutritious as fresh. Walking is free. Bodyweight exercises like squats and push-ups need no equipment. Many community centers offer free or low-cost fitness classes. Focus on what you can do today-not what you can’t.
Is it too late to make changes if I’ve been on meds for years?
It’s never too late. Even people who’ve had type 2 diabetes for 15+ years have lowered their A1C and reduced insulin doses by changing their diet and activity levels. Your body responds to healthy habits at any age. Start where you are.
