Electronic prescribing was supposed to fix medication errors. It cut down messy handwriting, reduced wrong doses, and made refills easier. But instead of disappearing, transcription errors just changed shape. Now, instead of a doctor’s chicken scratch, you get a digital prescription that gets misread because one system doesn’t talk to another. A pharmacy tech spends 20 minutes a day fixing what should’ve been automatic. Patients get the wrong medicine. Or worse-they don’t get it at all.
Why E-Prescribing Still Causes Transcription Errors
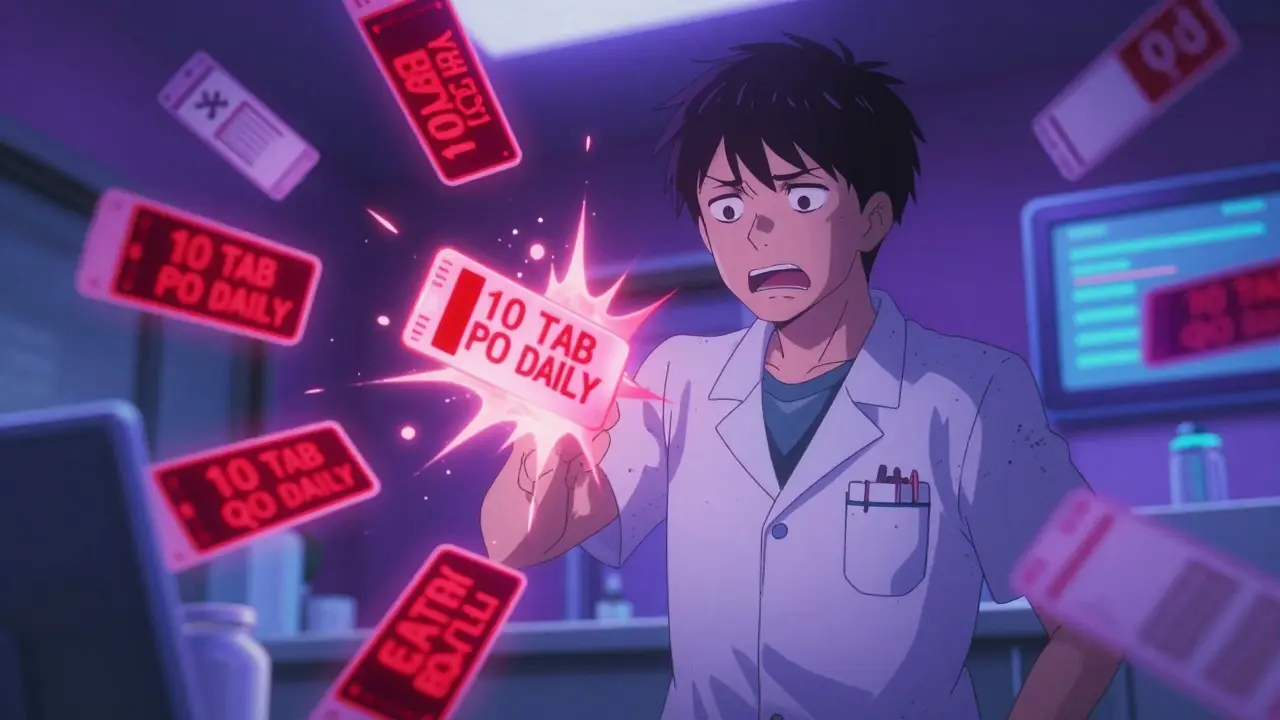
E-prescribing systems were designed to eliminate human mistakes. But they didn’t remove the human element-they just moved it. When a doctor’s EHR sends a prescription to a pharmacy’s system, the data doesn’t always arrive clean. Even though the prescription is digital, it often gets converted, reformatted, or re-entered manually because systems speak different languages. The biggest culprit? Incompatible formats. For example, a doctor’s system might send “take 1 tablet by mouth daily.” But the pharmacy’s system reads that as “1 TAB PO DAILY” and misinterprets it as “10 TAB PO DAILY.” That’s not a typo. That’s a system failure. A 2023 Reddit post from a pharmacy technician with over 800 upvotes described this exact issue: 27% of prescriptions from Epic EHRs to QS/1 pharmacy systems required manual correction because of garbled sigs. Another hidden problem: multiple prescriptions for the same drug. If a doctor changes a dose and sends a new e-prescription without canceling the old one, the pharmacy gets both. No way to tell which is correct. Pharmacists have to call the office. That’s not efficiency. That’s chaos.Structured Sig: The Simple Fix Most Practices Ignore
One of the most powerful tools to stop transcription errors isn’t fancy software. It’s standardizing how dosing instructions are written. This is called structured sig. Instead of free text like “take one pill every morning,” structured sig uses preset options: “1 tablet by mouth once daily.” Systems recognize these phrases. They don’t guess. They don’t misread. A 2018 Health Affairs study showed that adopting structured sig reduced transcription errors by 41% in pilot clinics. That’s not a small win. That’s life-saving. But most doctors still type free-form instructions because it’s faster. They don’t realize the cost. A 2021 AHRQ report found that 72% of practices resisted structured sig because it felt “burdensome.” But the real burden? The pharmacist calling back every other day because the system can’t read the sig. Training providers to use structured sig takes under five hours. The payoff? Fewer phone calls, fewer errors, fewer patients hurt.CancelRx: Stop the Confusion Before It Starts
Imagine you’re a pharmacist. Two e-prescriptions for the same patient arrive minutes apart: one for 5 mg of lisinopril, another for 10 mg. The doctor meant to change the dose. But didn’t cancel the first one. Now you have to track down the provider. That’s not just annoying. It’s dangerous. Enter CancelRx. Developed by Surescripts in 2012, this protocol lets prescribers electronically cancel a previous prescription. When a new one is sent, the old one disappears from the pharmacy’s queue. No confusion. No guesswork. A 2020 AHRQ review found that practices using CancelRx reduced discontinued medication errors by 63%. Yet, only 48% of U.S. practices use it. Why? Many EHRs don’t enable it by default. Or the doctor doesn’t know it exists. The fix? Make CancelRx mandatory in your EHR settings. Train every prescriber to use it every time they change a dose. No exceptions.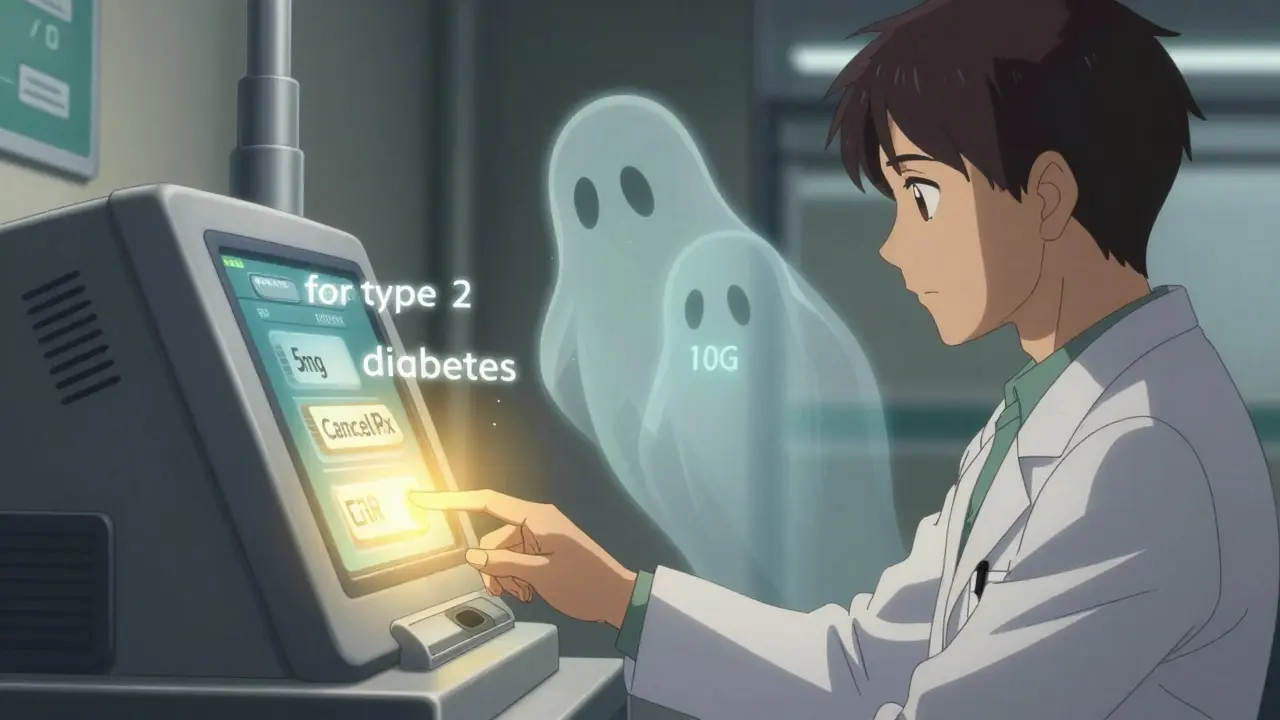
Interoperability Isn’t Optional-It’s the Foundation
You can’t fix transcription errors if your EHR doesn’t talk to your pharmacy system. That’s not a bug. It’s a design flaw. The solution? Interoperability standards. The gold standard today is HL7 FHIR (Fast Healthcare Interoperability Resources). FHIR lets systems exchange data like apps share photos-clean, fast, no translation needed. A 2017 ISMP Canada case study showed FHIR eliminated 92% of manual re-entry errors. That’s not theoretical. That’s real. CVS and Epic systems using FHIR saw near-zero transcription errors in their 2022 MGMA case study. But most small practices still use standalone e-prescribing tools like DrFirst Rcopia. These are cheaper and easier to set up. But they don’t connect to EHRs. That means the doctor has to copy-paste patient info from one screen to another. That’s where errors creep in. A 2019 KLAS report found standalone systems had 42% fewer transcription errors than EHR-integrated ones-but only because integrated systems were poorly configured. The real difference? When EHR and pharmacy systems are fully connected, transcription errors drop by 67%. The bottom line: If you’re not using FHIR or a certified integrated system, you’re still doing manual work. And manual work = human error.Medication Indications: The Silent Error Killer
Here’s a hidden danger: doctors prescribe metformin for diabetes. But the system doesn’t know why. So when a patient’s kidney function drops, the pharmacist sees “metformin 500 mg daily” and wonders: Is this still safe? Should it be stopped? No context. No clarity. Dr. David Bates from Harvard found that adding the reason for the prescription-like “for type 2 diabetes”-cuts dosing errors by 78%. Why? Because the system can now flag unsafe matches. If a patient has chronic kidney disease, and the prescription says “metformin for diabetes,” the pharmacy system can alert: “Metformin contraindicated in CKD Stage 3+.” That’s not a warning. That’s protection. Yet, only 19% of EHRs currently capture medication indications. It’s not hard. Just add a dropdown: “Hypertension,” “Diabetes,” “Pain,” “Infection.” But most providers skip it. They think it’s extra work. They don’t realize it’s the difference between a pharmacist calling and a patient going to the ER.
What You Can Do Today
You don’t need a $500,000 upgrade to fix this. Start with these six steps:- Turn on structured sig in your EHR. Make it required. No free text allowed.
- Enable CancelRx for every prescriber. Train them to use it every time they change a dose.
- Add medication indications as a mandatory field. Use preset options.
- Verify your EHR connects to your pharmacy via FHIR or NCPDP SCRIPT 201900. If it doesn’t, demand it.
- Train pharmacists on new error flags. They’re your first line of defense.
- Use the Surescripts Pharmacy Health Information Exchange if your system supports it. It cut errors by 88% in pilots.
Why This Matters More Than You Think
Transcription errors aren’t just paperwork problems. They’re patient safety issues. A 2003 study by Kaushal et al. showed e-prescribing dropped errors from 42.5 per 100 prescriptions to 6.6 per 100. But even that 6.6 includes transcription errors. That’s still one mistake every 15 prescriptions. The 21st Century Cures Act made it illegal for systems to block data exchange. The DEA now requires electronic prescriptions for controlled substances. CMS penalizes practices that don’t e-prescribe. But none of that matters if the data arrives broken. The future is here. AI tools like Epic’s DoseMeRx are entering pilot phase in 2023 and could reduce transcription errors by another 65% by 2026. But they won’t work if your systems don’t talk. FHIR adoption is the key. And by 2025, the ONC will require it. Waiting isn’t an option. Every day you delay, a pharmacist is still guessing. A patient is still at risk. Fixing transcription errors isn’t about technology. It’s about discipline. It’s about choosing safety over speed. And it starts with one setting. One click. One change.What’s the most common cause of transcription errors in e-prescribing?
The most common cause is incompatible data formats between prescriber EHRs and pharmacy systems. For example, a prescription written as “take 1 tablet daily” might be converted to “1 TAB PO DAILY,” which some pharmacy systems misread as “10 TAB PO DAILY.” This happens in 27% of prescriptions from Epic to QS/1 systems, according to pharmacy staff reports.
Can e-prescribing systems cancel old prescriptions automatically?
Yes, through the CancelRx protocol, which lets prescribers electronically cancel previous prescriptions when updating a medication. When used correctly, CancelRx reduces discontinued medication errors by 63%. However, only 48% of practices use it, often because it’s not enabled by default in their EHR.
Do I need to upgrade my EHR to fix transcription errors?
Not necessarily. Many errors can be fixed with configuration changes: enabling structured sig, turning on CancelRx, adding medication indications, and ensuring your system uses the NCPDP SCRIPT 201900 standard. Upgrading to a fully integrated FHIR-based system (like Epic or Cerner with direct pharmacy connectivity) reduces errors by 67%, but basic fixes can cut errors by 40% without new software.
Why do some small practices have fewer transcription errors than large hospitals?
Small practices using standalone e-prescribing tools like DrFirst Rcopia often have fewer errors because they avoid the complexity of integrating with full EHRs. But this is misleading: integrated systems like Epic reduce overall prescribing errors by 84%. The real issue is poor configuration. When EHRs are poorly connected to pharmacies, errors rise-even in large hospitals. The difference isn’t size-it’s how well the system is set up.
How long does it take to implement these fixes?
You can implement the top three fixes-structured sig, CancelRx, and medication indications-in under 12 weeks. Training providers takes about 4.7 hours per person. Pharmacists need 3.2 hours to adapt to new error alerts. Most practices can complete this without external help, though 15% require consultants for system configuration.
Is FHIR really that important for e-prescribing?
Yes. FHIR is the only standard that allows true interoperability-no manual re-entry, no format conversion. A 2017 ISMP Canada study showed FHIR eliminated 92% of transcription errors. The ONC mandates FHIR-based e-prescribing by 2025. Systems not using FHIR will become obsolete. If your system doesn’t support it, ask your vendor when it will.
Can AI help reduce transcription errors in the future?
Yes. AI tools like Epic’s DoseMeRx, currently in pilot phase, analyze prescriptions for safety based on patient history, lab results, and drug interactions. Early results show they can reduce transcription errors by an additional 65% by 2026. But AI can’t fix broken data. It needs clean, structured input from interoperable systems. Without FHIR and standardized sigs, AI won’t work as intended.