It’s 3 a.m. in a rural emergency room. A patient is having a heart attack. There are two nurses on duty. One is already caring for three other critical patients. The other just finished a 16-hour shift. The doctor on call is stuck in traffic. The ambulance outside is waiting 90 minutes to offload because the ER is full. This isn’t fiction. It’s happening right now in over 40 U.S. states.
Why Hospitals and Clinics Are Struggling to Stay Open
The problem isn’t just one thing. It’s a chain reaction. Fewer nurses, fewer doctors, fewer support staff. And the people who are still working are burned out, exhausted, and leaving in droves. In 2024, nearly 63% of nurses said they were thinking about quitting because of unsafe patient loads. That’s not just a statistic-it means hospitals are losing staff faster than they can hire them. The numbers tell the story. By 2030, the U.S. will be short more than 500,000 registered nurses. That’s not a guess. It’s a projection from the Health Resources and Services Administration. And it’s not just nursing. There’s a looming shortage of 86,000 physicians by 2036. Meanwhile, over half of all nurses are over 50. That means a huge wave of retirements is coming-and there aren’t enough new graduates to replace them. Rural clinics are hit hardest. They’re operating at just 58% staffing levels, compared to 79% in urban areas. In places like rural Nevada or eastern Kentucky, clinics have closed entire wings because they can’t find staff. Some hospitals have had to shut down 12 inpatient beds every week just to stay within safe staffing rules. That’s $4 million a month in lost revenue-and more importantly, it’s patients who can’t get care when they need it.What Happens When There’s No One to Care for You
When staff numbers drop, patient outcomes drop with them. Studies show that when a nurse is responsible for more than four patients, the risk of death increases by 7%. That’s not a small margin. That’s life or death. Emergency departments now see wait times that are 22% longer than they were in 2022. In some places, patients are waiting 72 hours just to be seen. Medication errors are climbing. ICU nurse Sarah Chen, who posted on Reddit about her experience in 2025, said she had two near-miss errors last month because she was managing three critically ill patients alone. That’s not negligence. That’s a system pushed past its breaking point. Long-term care facilities are in even worse shape. They’re operating with 28% fewer nurses than before the pandemic. Elderly patients who need help bathing, eating, or turning in bed are going hours without assistance. Infections are spreading. Families are seeing their loved ones deteriorate because there’s no one to monitor them. Behavioral health is collapsing. There are 12,400 unfilled positions in mental health and substance abuse services across the country. People having panic attacks, suicidal thoughts, or psychotic episodes are being turned away because there’s no one to help them. Emergency rooms are becoming de facto mental health clinics-with no training, no resources, and no staff to handle it.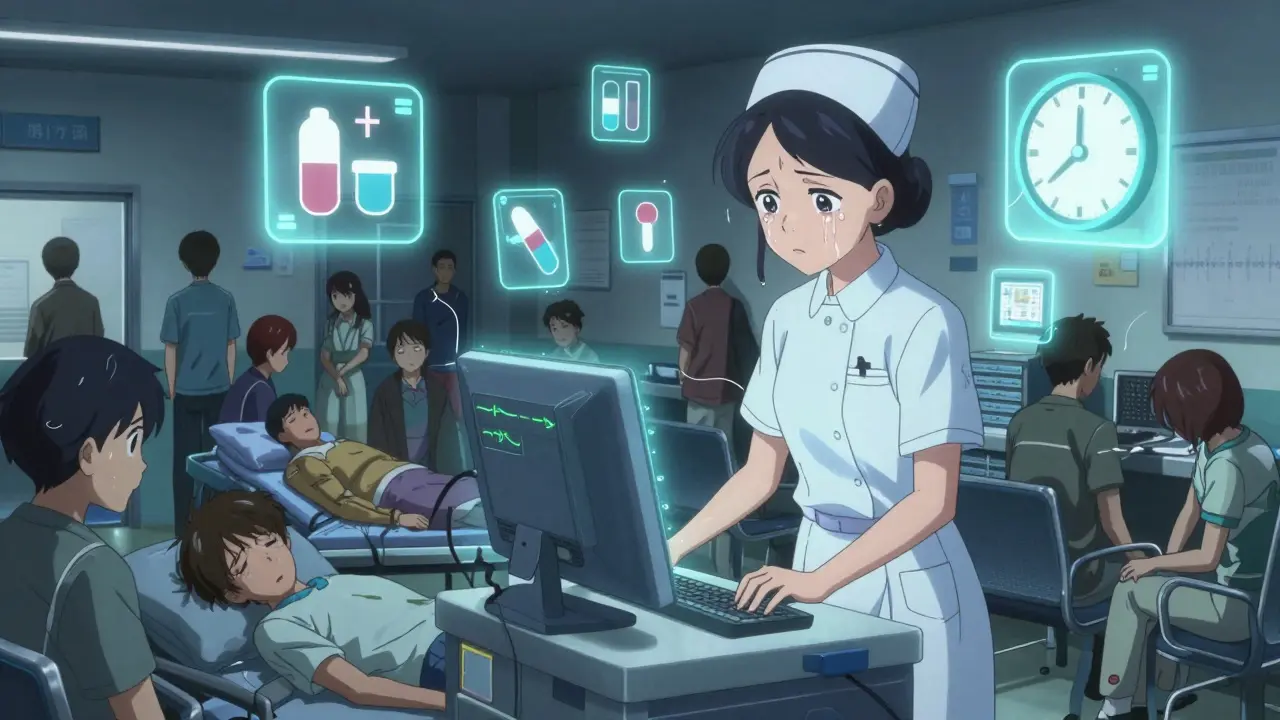
Why Travel Nurses Aren’t the Fix
Hospitals have tried to plug the gap with travel nurses. They’re paid up to $185 an hour in places like New York City-more than three times what a permanent staff nurse makes. That sounds like a solution. But it’s not. Travel nurses fill 12% of hospital roles, but they cost 34% more in labor. That money comes out of budgets meant for equipment, training, or hiring permanent staff. And when the travel nurse leaves, the problem is still there. Meanwhile, the nurses who stayed behind are watching their coworkers earn triple their pay while doing the same job. Resentment grows. Morale plummets. Some hospitals have turned to AI and telehealth to reduce the burden. One pilot program cut ER visits by 19% using virtual nurse triage. But it cost $2.3 million to set up. And 68% of hospitals can’t even get their electronic health records to talk to each other, let alone integrate new tech. Training staff to use AI tools takes 32 hours per person-and most nurses don’t have that kind of time.The Real Problem: No One’s Fixing the Root Cause
The system is treating symptoms, not the disease. Loan forgiveness programs in states like Massachusetts have helped reduce shortages to 8% below the national average. But federally, nursing education gets only $247 million a year. Experts say it needs $1.2 billion. That’s a gap of nearly $1 billion. Nursing schools are turning away 2,305 qualified applicants every year-because there aren’t enough faculty to teach them. And why? Because experienced nurses can make more money working in a hospital than teaching. So the pipeline dries up. States are starting to act. California now requires a 1:5 nurse-to-patient ratio in medical-surgical units. Other states are following. But without national funding, consistent standards, and real investment in training, these rules are just paper promises. The Biden administration pledged $500 million for nursing education in April 2025. That sounds like a lot. But it covers just 18% of what’s actually needed. The American Hospital Association says it will take $22 billion in targeted investment over the next five years to even start closing the gap.
What’s Next? The System Is at a Crossroads
If nothing changes, the crisis will keep getting worse. By 2027, the global shortage of healthcare workers could hit 15 million. In the U.S., rural hospitals will keep closing. Urban ERs will stay overwhelmed. Older adults won’t get the care they need. And more nurses will quit. But there’s a path forward. It’s not simple. It’s not cheap. But it’s possible. We need to pay nurses what they’re worth-not just in salary, but in respect. We need to fund nursing schools so they can hire more teachers and admit more students. We need to give hospitals the tools to use AI and automation without breaking their budgets. We need to remove state licensing barriers that stop nurses from working across borders. Most of all, we need to stop treating this as a temporary crisis. It’s not. It’s the result of decades of underinvestment, poor working conditions, and broken policies. The people who show up every day to care for us are exhausted. And if we don’t act now, we’ll wake up one day to find the system gone.What You Can Do
You don’t have to be a policymaker to help. Talk to your representatives. Ask them what they’re doing about nurse shortages. Support local clinics with donations or volunteer time. If you’re in healthcare, speak up about unsafe conditions. If you’re a student, consider nursing or medical school-even if the pay seems low now, the need is real and growing. The healthcare system isn’t broken because of bad luck. It’s broken because we stopped caring enough to fix it. It’s time to change that.Why are hospitals closing beds due to staffing shortages?
Hospitals close beds when they don’t have enough nurses or doctors to safely care for patients. Regulations require minimum nurse-to-patient ratios-like 1:4 or 1:5-depending on the unit. If a hospital can’t meet those ratios, they legally can’t open more beds. This isn’t a choice-it’s a safety rule. In 2024, some hospitals closed 12 beds per week just to stay compliant.
Are travel nurses making the shortage worse?
Travel nurses help fill gaps, but they don’t solve the problem. They’re expensive-costing hospitals 34% more than permanent staff. That money could be used to hire full-time workers or improve working conditions. Plus, when travel nurses leave, the vacancy returns. Many permanent staff feel resentment seeing travel nurses earn triple their pay for the same work, which lowers morale and drives more people out.
Why are rural clinics hit harder than urban ones?
Rural clinics have fewer applicants for every job, lower pay, and less access to training or support. They also serve older populations with higher healthcare needs. As a result, rural clinics operate at just 58% staffing, compared to 79% in urban clinics. Many have shut down entire departments or stopped taking new patients because they can’t find staff.
How do nurse shortages affect patient safety?
When nurses are overworked, mistakes happen. Studies show that for every additional patient added to a nurse’s load, the risk of death increases by 7%. Longer wait times, missed medications, delayed responses-all become common. In 2024, 41% of nurses reported considering leaving the profession because of unsafe patient ratios.
Is technology like AI going to solve the staffing crisis?
AI can help-by automating documentation, triaging patients, or monitoring vitals remotely. But it’s not a magic fix. Only 28% of hospitals say AI tools have improved retention. Training staff takes weeks. Systems often don’t talk to each other. And AI can’t replace human compassion or judgment. It’s a tool, not a replacement.
What’s being done to train more nurses?
Nursing schools are turning away over 2,300 qualified applicants each year-not because they lack interest, but because they lack faculty. Experienced nurses make more money working in hospitals than teaching. Federal funding for nursing education is $247 million a year, but experts say $1.2 billion is needed. Without more teachers, there won’t be enough new nurses to fill the gap.
