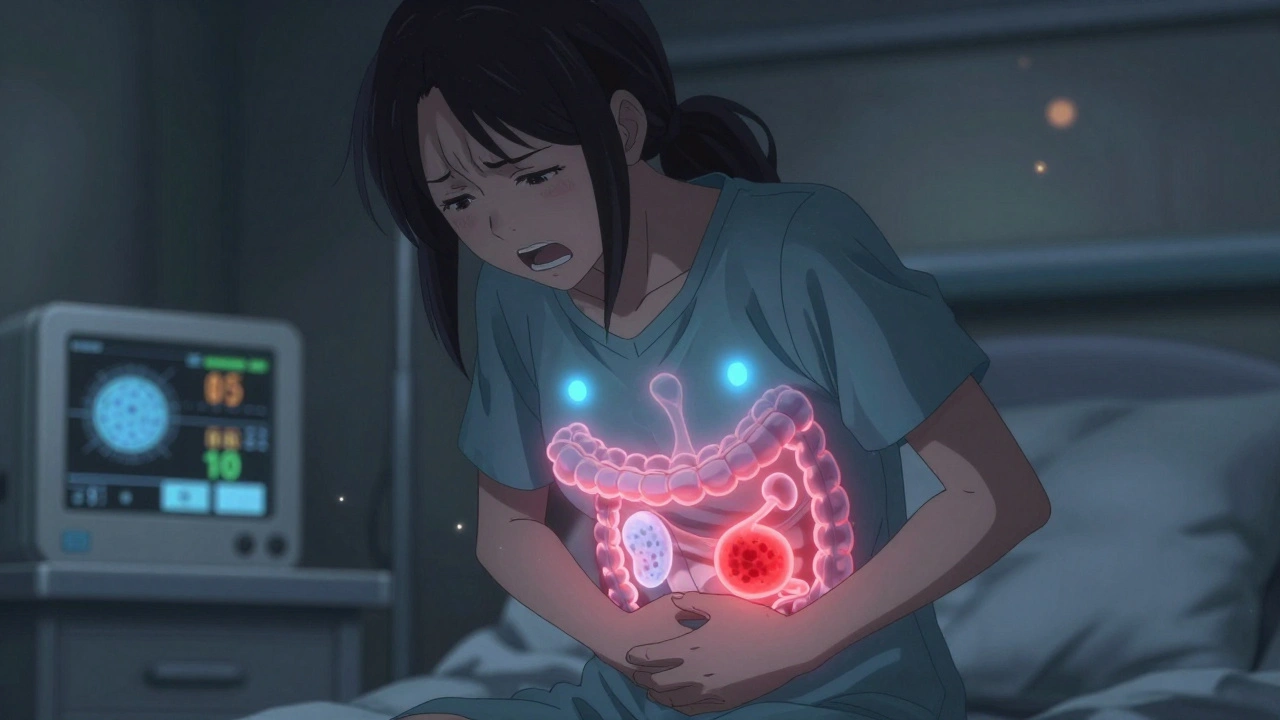
When you feel a sharp, constant pain in your lower left abdomen, along with fever and nausea, it’s easy to assume it’s just a bad stomach bug. But if this pain keeps coming back or doesn’t improve with rest, it could be something more specific: diverticulitis. This isn’t just a passing discomfort-it’s inflammation in small pouches that have formed in your colon wall. These pouches, called diverticula, are common as we age, but when they get infected or irritated, they turn into a medical issue that can disrupt your life for weeks-or even lead to surgery.
What Exactly Are Diverticula?
Diverticula are tiny, balloon-like bulges that push out through weak spots in the muscle layer of your colon. They’re not tumors, not polyps, and not caused by eating seeds or nuts. They’re simply the result of pressure building up inside your colon over time. Think of it like a balloon with a thin spot-it bulges where the wall is weakest. In most people, these pouches never cause trouble. That’s called diverticulosis, and by age 60, more than half of adults have them. But when bacteria get trapped inside one of these pouches, or the pouch tears slightly, inflammation follows. That’s diverticulitis.Over 95% of these pouches form in the sigmoid colon-the S-shaped part of the colon just before the rectum. That’s why the pain is almost always on the lower left side. But in people of Asian descent, right-sided diverticulitis is more common due to differences in colon structure. The pouches themselves are small, usually between 5 and 10 millimeters, but their impact can be huge.
How Do You Know It’s Diverticulitis and Not Something Else?
The symptoms can look a lot like other gut problems. Irritable bowel syndrome (IBS) causes bloating and cramps. Appendicitis causes right-sided pain. Kidney stones bring sharp, intermittent pain. But diverticulitis has a signature pattern:- Constant, localized pain in the lower left abdomen (or sometimes right, depending on anatomy)
- Fever above 38°C (100.4°F)
- Nausea or vomiting
- Changes in bowel habits-constipation or diarrhea
- Pain that gets worse when you move or cough
What makes it different from IBS? IBS pain is crampy, comes and goes, and doesn’t cause fever. Diverticulitis pain is steady, often severe, and usually comes with a fever and elevated white blood cell count. In fact, 70-80% of diverticulitis patients have a fever. If you’re told your bloodwork is normal but you’re still in pain, don’t assume it’s all in your head. Studies show nearly a quarter of diverticulitis cases are misdiagnosed the first time, especially in women who are told it’s an ovarian cyst.
Doctors rely on a CT scan to confirm it. The scan shows inflamed pouches, thickened colon walls, and sometimes small abscesses. A simple physical exam and blood test aren’t enough. A CT scan costs between $1,200 and $1,800, but skipping it can lead to worse outcomes-and cost you more in the long run if you end up with a perforation or emergency surgery.
How Serious Is It? The Hinchey Staging System
Not all cases of diverticulitis are the same. Doctors use the Hinchey classification to figure out how bad it is:- Stage Ia: Small, localized inflammation around one pouch. No abscess.
- Stage Ib: A small abscess (less than 3 cm) forms near the pouch.
- Stage II: A larger abscess (3-5 cm) in the pelvis.
- Stage III: Pus spreads into the abdominal cavity but doesn’t leak feces.
- Stage IV: A hole forms in the colon, and stool leaks into the belly. This is a medical emergency.
Most people (about 75%) fall into Stage I or II. These are usually treated without surgery. But Stage III and IV require immediate hospitalization-and often surgery. The good news? Most people don’t reach that point if they get diagnosed early.
The Big Shift in Treatment: Antibiotics Aren’t Always Needed
Ten years ago, if you had diverticulitis, you got antibiotics-no questions asked. Today, that’s changed. A major study called the DIVERT trial, published in the New England Journal of Medicine in 2021, showed that for mild, uncomplicated cases, antibiotics didn’t speed up recovery. Patients who rested, drank fluids, and took pain relief did just as well as those who took amoxicillin-clavulanate.Now, doctors follow a simple rule: if you’re otherwise healthy, your fever is below 38.5°C, your blood work isn’t wildly abnormal, and your CT scan shows only mild inflammation-you probably don’t need antibiotics. Your body can fight it off on its own. Instead, you’re told to:
- Stay on clear liquids for 48-72 hours
- Gradually add low-fiber foods like white rice, eggs, and cooked vegetables
- Take acetaminophen (Tylenol) for pain-avoid NSAIDs like ibuprofen, which can increase the risk of perforation
But if you have a high fever, severe pain, or a weakened immune system, antibiotics are still essential. Common choices include amoxicillin-clavulanate, ciprofloxacin with metronidazole, or piperacillin-tazobactam for hospitalized patients. The goal isn’t to kill every last bacterium-it’s to prevent the infection from spreading.
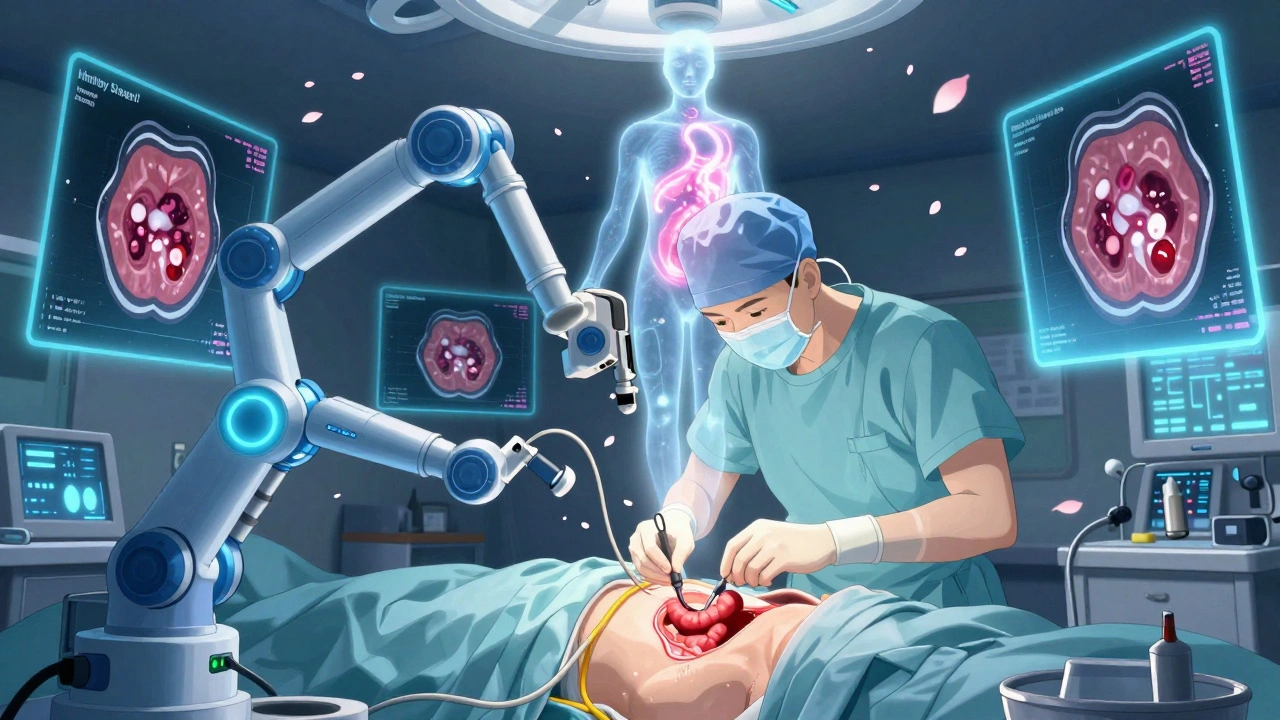
What About Surgery?
Surgery used to be common after two or three attacks. Now, the guidelines have changed. The American Society of Colon and Rectal Surgeons says to consider surgery after just two attacks-especially if you’ve been hospitalized each time. Why? Because between attacks, many people live with chronic pain, bloating, and fear of the next flare-up. One patient on Reddit described it as “living on a knife’s edge.”Surgery usually means removing the affected part of the colon-the sigmoid colon. Laparoscopic surgery (keyhole) is standard now. Recovery takes about 4-6 weeks. In complicated cases like Stage III or IV, surgeons may do a laparoscopic lavage (cleaning out the abdomen) instead of removing the colon right away. The 2022 SCANDIV trial showed this approach worked in 82% of cases, avoiding a permanent colostomy.
After an attack, whether mild or severe, you’ll need a colonoscopy 6-8 weeks later. Why? Because diverticulitis can mask colon cancer. A 2021 JAMA study found that 1.3% of patients over 50 with diverticulitis had cancer hiding behind the inflammation. That’s why the scan isn’t optional-it’s a safety net.
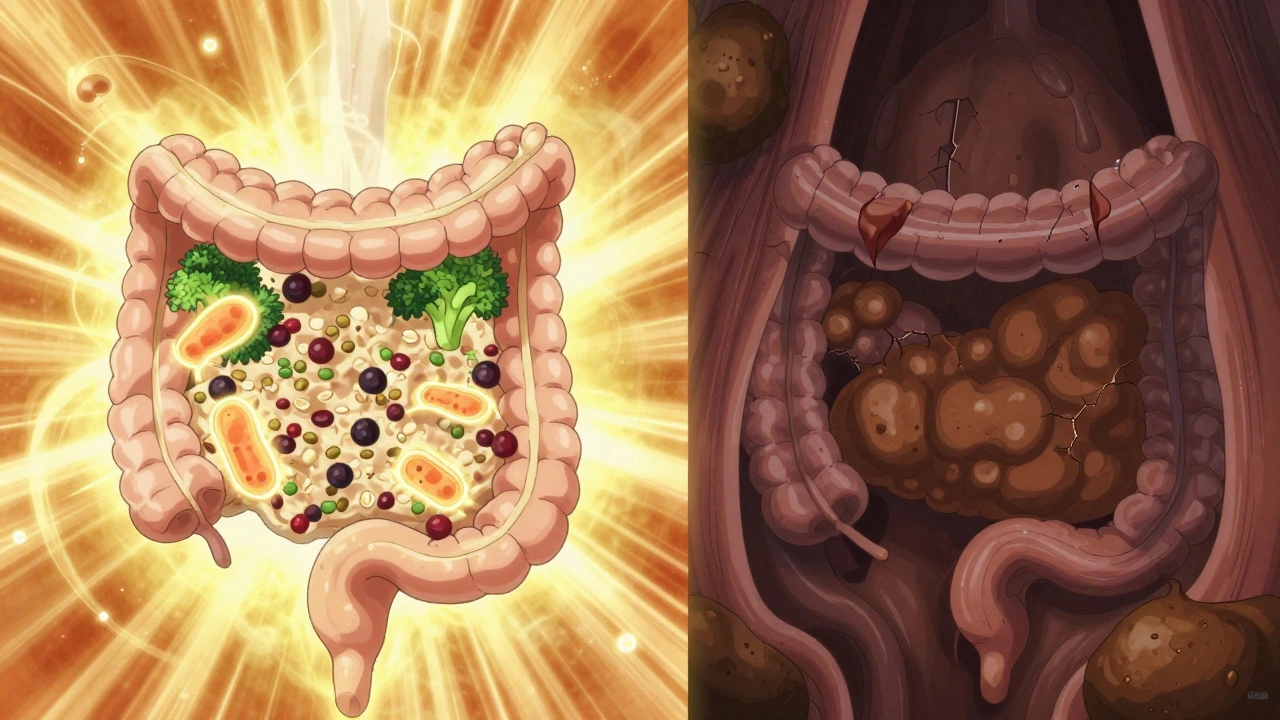
Preventing the Next Attack: Diet, Lifestyle, and New Hope
The biggest question after recovery is: “Will this happen again?” About 15-30% of people have a second episode. But you can lower that risk.For years, doctors told people to avoid nuts, seeds, popcorn, and corn. That advice came from old assumptions, not science. In 2021, a massive 18-year study of 47,000 women in the Nurses’ Health Study found no link between eating these foods and diverticulitis. In fact, those who ate more nuts and seeds had slightly lower rates of attacks.
What does matter? Fiber. A diet low in fiber leads to harder stools, which means more pressure in the colon. That pressure creates the weak spots where diverticula form. The goal is 30-35 grams of fiber daily. That means:
- Whole grains (oats, quinoa, brown rice)
- Legumes (beans, lentils, chickpeas)
- Vegetables (broccoli, Brussels sprouts, carrots)
- Fruits (apples, pears, berries)
One patient shared on MyCrohnsAndColitisTeam that after his second attack, he increased his fiber to 35 grams a day-and went 27 months without another flare-up.
Other lifestyle changes help too:
- Quit smoking-smokers have nearly 3 times the risk
- Exercise at least 2 hours a week-sedentary people have 38% higher risk
- Maintain a healthy weight-BMI over 30 doubles your risk
New treatments are on the horizon. In 2023, the FDA approved mesalazine (Pentasa®) for maintenance therapy after an attack. In trials, it cut recurrence by 31% over 12 months. Researchers are also looking at the gut microbiome. Patients with diverticulitis often have lower levels of Faecalibacterium prausnitzii, a good bacterium that helps reduce inflammation. Future treatments might involve targeted probiotics or fecal transplants.
Even AI is stepping in. Mayo Clinic has developed a tool that looks at your CT scan, blood results, age, and BMI to predict your risk of another attack-with 83% accuracy. That means doctors can now personalize prevention plans instead of guessing.
The Hidden Cost: Time, Money, and Quality of Life
Diverticulitis isn’t just a medical issue-it’s a life disruptor. In the U.S., it leads to 200,000 hospitalizations a year and costs $2.3 billion. But the real cost? The time lost. One patient reported missing three weeks of work after his first attack-even though his bloodwork was normal. Another said he spent six months seeing five different doctors before getting the right diagnosis.Patients who get treated early and avoid complications rate their satisfaction at 4.2 out of 5. But those who end up in the hospital for a complicated case rate it at just 2.8. The difference? Early action. Listening to your body. Not ignoring pain that doesn’t go away.
Diverticulitis is common. It’s treatable. And with the right approach, it doesn’t have to define your life. You don’t need to live in fear of your next meal. You don’t need to avoid nuts or seeds. You just need to eat more fiber, move more, quit smoking, and get checked when something feels off.
The era of overtreating diverticulitis is over. The era of underestimating it? That’s still happening. Don’t be the one who waits too long.
Can diverticulitis go away without antibiotics?
Yes, for mild, uncomplicated cases, diverticulitis can resolve on its own with rest, hydration, and a clear liquid diet followed by a low-fiber diet. Studies like the 2021 DIVERT trial show no difference in recovery time between patients who took antibiotics and those who didn’t. Antibiotics are now reserved for cases with fever above 38.5°C, high white blood cell counts, or signs of worsening infection.
Are nuts and seeds dangerous if you have diverticulitis?
No. This is an outdated myth. A large 18-year study of 47,000 women found no increased risk of diverticulitis from eating nuts, seeds, or popcorn. In fact, those who ate more of these foods had slightly lower rates of flare-ups. Current guidelines encourage including them as part of a high-fiber diet.
When should you go to the ER for diverticulitis?
Go to the ER if you have severe, worsening abdominal pain; a fever over 38.5°C (101.3°F); vomiting that won’t stop; dizziness or rapid heartbeat; or signs of shock like cold, clammy skin. These could indicate a perforation, abscess, or peritonitis-serious complications that need immediate treatment.
Do you need surgery after multiple diverticulitis attacks?
Surgery isn’t automatic after every attack. But if you’ve had two or more attacks that required hospitalization, or if you’re living with ongoing pain and reduced quality of life between episodes, surgery to remove the affected part of the colon (usually the sigmoid) may be recommended. The decision is based on frequency, severity, and how much it affects your daily life-not just the number of attacks.
Why do you need a colonoscopy after diverticulitis?
Diverticulitis can hide colon cancer. Inflammation and scarring make it hard to see tumors on a CT scan. A colonoscopy, done 6-8 weeks after the infection clears, checks for polyps or cancer. Studies show about 1.3% of patients over 50 with diverticulitis have an undiagnosed cancer-making this test essential for safety.
Can diverticulitis come back even after surgery?
If the affected part of the colon is removed, the risk of recurrence in that area drops to nearly zero. However, new diverticula can form in other parts of the colon, though this is rare. Most patients who have surgery don’t experience another attack. Lifestyle factors like diet and exercise still matter to keep the rest of the colon healthy.
What Comes Next?
If you’ve had one episode, focus on prevention: increase fiber slowly, drink plenty of water, stay active, and avoid smoking. Keep track of your symptoms. If pain returns, don’t wait. See your doctor early. If you’re still unsure what to eat, start with a simple plan: oatmeal for breakfast, a lentil salad for lunch, steamed broccoli and brown rice for dinner. Add an apple or pear. That’s over 25 grams of fiber right there.Diverticulitis isn’t a death sentence. It’s a signal. A sign that your colon needs better fuel and less pressure. With the right changes, most people never have a second attack. And if they do, modern medicine has more tools than ever to help them through it-without unnecessary antibiotics, without emergency surgery, without fear.