Anticholinergic Burden Calculator
Calculate Your Anticholinergic Burden
The Anticholinergic Cognitive Burden (ACB) scale rates medications from 0 (no anticholinergic activity) to 3 (strong anticholinergic activity). Total score is the sum of all drugs you take. A score of 2 or higher increases dementia risk.
Your Anticholinergic Burden Assessment
What does this mean?
Select medications to see your assessment.
For decades, millions of older adults have reached for over-the-counter antihistamines like Benadryl to help them sleep or manage allergies. But new research is raising serious questions about whether these common pills might be quietly damaging brain health over time. The concern isn’t about a single dose-it’s about years of use. And it’s not just a theory. Major medical organizations now warn that certain antihistamines may increase dementia risk in older adults. The truth is more complicated than it sounds, but if you or a loved one is taking these meds regularly, you need to understand the real risks-and what to do instead.
Not All Antihistamines Are the Same
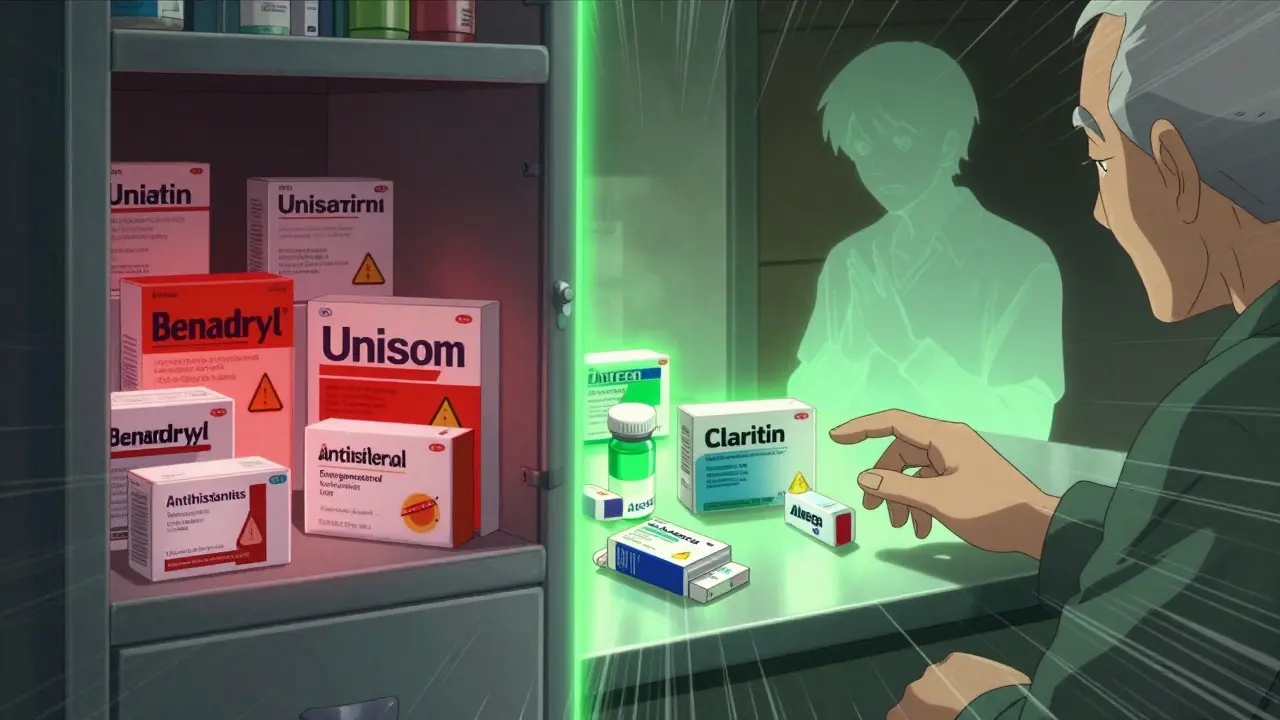
There are two main types of antihistamines: first-generation and second-generation. The difference isn’t just in brand names-it’s in how they affect your brain.First-generation antihistamines like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine cross the blood-brain barrier easily. They block acetylcholine, a chemical your brain needs for memory, focus, and learning. This is why they make you drowsy-and why they’re often used as sleep aids. But that same effect can be dangerous over time. These drugs are classified as strong anticholinergics, meaning they interfere with a key brain signaling system.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed to avoid this. They don’t cross into the brain as easily. They’re just as effective for allergies, but they don’t carry the same brain-related risks. In fact, their anticholinergic activity is 100 to 1,000 times weaker than first-gen versions. If you’re taking an antihistamine daily, switching to a second-generation option could cut your risk dramatically.
The Science Behind the Warnings
A landmark 2015 study in JAMA Internal Medicine followed over 3,400 adults aged 65 and older for 10 years. It found that people who took strong anticholinergic drugs-including certain antidepressants, bladder medications, and first-gen antihistamines-had a higher risk of developing dementia. The more they took, and the longer they took them, the greater the risk.But here’s where it gets tricky: later studies showed mixed results. A 2022 analysis of nearly 9,000 older adults found no statistically significant link between antihistamine use and dementia. The same study found that people taking second-gen antihistamines had dementia rates of just 1%, compared to 3.8% in those using first-gen versions. But the difference wasn’t strong enough to prove causation.
Another 2019 study looked specifically at antihistamines and found no increased dementia risk (hazard ratio of 1.00). That’s surprising, given how often they’re used. But when researchers grouped all anticholinergic drugs together-including powerful bladder meds and antidepressants-they found a 46% higher risk. That suggests antihistamines alone might not be the main culprit. But they’re still part of the problem.
The American Geriatrics Society’s 2023 Beers Criteria, which guides doctors on safe prescribing for older adults, gives first-gen antihistamines a clear “Avoid” rating. That’s the strongest warning level. The European Medicines Agency is more cautious, calling the evidence “inconsistent,” but still recommends updated warnings on labels about long-term cognitive effects.
Why Do Experts Still Worry?
Even if the data isn’t perfectly clear, many doctors still advise caution. Why? Because the brain doesn’t recover easily from long-term acetylcholine suppression. Think of it like turning down the volume on your radio for years-you might not notice the difference right away, but eventually, the signal gets fuzzy.Dr. Shelley Gray, lead author of the original 2015 study, says the strongest links are with antidepressants and bladder meds, not antihistamines. But she also says: “We can’t ignore the fact that millions of older adults are using these drugs every night.”
Dr. Malaz Boustani, a dementia researcher, points out that older adults often take multiple medications. Even a small anticholinergic burden from one drug can add up. If someone is also taking a stomach acid reducer, a painkiller, or a sleep aid-all of which can have anticholinergic effects-the total load becomes dangerous. That’s why the Anticholinergic Cognitive Burden Scale (ACB) rates diphenhydramine as a level 3-the highest risk. Fexofenadine? Level 0. No risk.
And it’s not just about dementia. First-gen antihistamines are linked to confusion, falls, urinary retention, and constipation in older adults. These side effects are often mistaken for “normal aging.” They’re not.
What People Are Really Using-and Why
Despite the warnings, first-gen antihistamines are still everywhere. In 2022, they made up 62% of the $874 million over-the-counter sleep aid market. Many people don’t realize they’re taking an anticholinergic. The label says “helps you sleep” or “allergy relief,” not “may damage your memory.”A 2022 survey by the National Council on Aging found that 42% of adults over 65 use OTC antihistamines for sleep. And 78% had no idea these drugs carry brain risks. On Reddit, users in r/geriatrics report that 83% of their elderly clients take Benadryl nightly-often because their doctor prescribed it years ago, and no one ever told them to stop.
One woman on AgingCare.com wrote: “My mother’s doctor prescribed Benadryl for years to help her sleep, and now she has dementia. I can’t help but wonder if there’s a connection.” She’s not alone. Thousands of families are asking the same question.

What Should You Do Instead?
If you’re taking diphenhydramine or doxylamine regularly, don’t quit cold turkey. Talk to your doctor. But here’s what you can do right now:- Switch to a second-generation antihistamine. Claritin, Zyrtec, or Allegra work just as well for allergies and don’t affect your brain.
- For sleep, try non-drug options. Cognitive Behavioral Therapy for Insomnia (CBT-I) works better than pills for older adults. Studies show 70-80% success rates. The catch? Therapists are hard to find, and Medicare pays only $85-$120 per session.
- Ask about Silenor. This prescription sleep aid (low-dose doxepin) has minimal anticholinergic effects and is approved for long-term use. It’s not cheap, but it’s safer than Benadryl.
- Review all your meds. Use the ACB scale to check if other drugs you take-like antacids, pain relievers, or bladder meds-also carry anticholinergic risk. Add them up. Even small doses can pile up.
- Ask your doctor to reassess every six months. The American Academy of Neurology recommends regular medication reviews. Just because a drug was prescribed years ago doesn’t mean you still need it.
The Choosing Wisely campaign, backed by the American Board of Internal Medicine, lists “avoiding diphenhydramine for chronic insomnia in older adults” as one of its top five recommendations for safe care. That’s not a suggestion-it’s a standard.
What’s Next?
A major new study called ABCO, launched in January 2023 with $4.2 million in NIH funding, is tracking 5,000 adults over 10 years to get clearer answers. Early data from the UK Biobank suggests that when researchers control for underlying sleep disorders, antihistamine use doesn’t raise dementia risk. That could mean the real problem isn’t the drug-it’s the reason people take it: poor sleep, which itself is linked to cognitive decline.The FDA is reviewing all anticholinergic medications and expects to release findings in mid-2024. Meanwhile, drugmakers are shifting away from first-gen antihistamines. Global sales of diphenhydramine dropped 24% between 2015 and 2022. Sales of safer alternatives grew by 18%.
The message isn’t that all antihistamines are dangerous. It’s that the ones you’ve been using for years might be. And there are better, safer options waiting for you.
